Resumen
Índice
- Key Ideas
- Basic skills for listening
- Establishing a relationship: the impression the Doctor forms of the patient.
- Exploring part of the consultation: the semi-structured interview
- Importance of the first minute
- Delineating the presenting complaint. Map of demands and complaints. Pathobiography
- Exploring beyond the apparent presenting complaint
- Active listening 'the interview leak point' and the technique of 'pulling the thread”
- Textual reading and suggested addition techniques
- Framing and reframing the interview. Resistances.
- Mistakes to avoid
- Attitudinal errors
- Technical errors
- Situations gallery
- When listening hurts
- The patient with multiple complaints
- The intruding relative
- When the doctor and patient speak different languages
- Advanced concepts
- Types and purposes of listening
- Listening and emotions
- Good communication versus poor communication
- Therapeutic commitment
- The good listener
- The importance of non-verbal communication
- Time management
- Summary
- Bibliography
Listening to the patient
Key Ideas
-
Listening is predicting what will be said and being surprised when it does not match.
-
Only the curious listen well, others become bored ... and switch off!
-
Those who ask get answers, but only answers (Balint M, 1961).
-
Those who allow the patient to talk get stories.
-
In the first minutes of the interview, especially, if we let the patient talk, we may extract rough diamonds which may not re-emerge.
-
There is no possibility for empathy without developing patience.
-
Empathy, in contrast to the sympathy of friendships, maintains an emotional distance from the patient's suffering to enable better and fairer decisions.
-
Those who don’t know their areas of irritability are at the mercy of their negative emotions.
-
Hidden hostility and resentment in the doctor-patient relationship puts the doctor at risk of clinical errors.
-
Knowing a person is to discover the stereotype that we were applying and to dispel it!
-
Working out our “perplexity point” is to recognise that 'we don't know' what happens to the patient, and resist the temptation to deny this or conceal it with 'routine' solutions and to be aware we may need to look beyond the apparent presenting complaint.
Basic skills for listening
Our lives are the years we have lived, our experiences which have made us who we are, and the fortuity to have been born and be alive today rather than someone else. We have the task to understand others and to make ourselves understood, because to communicate is to share, but in doing so is to take a risk. Just sharing who we are is taking a risk.
What does one know about another person? Firstly, starting to know something about someone else is to question the information already known or which is thought to be known from to third parties and process the information for ourselves. Be open to surprise. The other person is a draft which needs to be confirmed in each visit, they are not a static picture. Knowing something about the patient also requires us to relearn our profession, because unlike a bank account, our knowledge doesn’t produce revenue. In a few years, if not months, the lazy clinician becomes an expert in prejudice. The idle person considers the patient from their own convenience, either trivialising their complaints or dogmatising what needs to be done or not done, in an attempt to remove the complexity of the situation and save themselves the effort of rethinking things. Because our expertise is not innate, it is always created from our current experiences, in the most recent months of our lives. Our continued expertise is built as a result of our continued will to excel in our field and, due to our desire to be the best of ourselves. Only those who reflect, or at least try to reflect on each clinical situation experienced, is a skilled and responsible professional because such reflection is a key principal of continued professional expertise. When we inevitably make a mistake, because we are human, the moral pain experienced, is mitigated by our deep conviction that we have properly considered the decisions taken.
On the other side, we have the professional who falters. The first phase is barely perceptible, and undoubtedly the most dangerous. Whatever happens is not that one suddenly thinks: 'today I stop being a good professional'. Of course not. The first imperceptible step is the step toward mediocrity. Mediocrity does not consist of doing things wrong, but of not wanting to do things better. The professional who slides into mediocrity says to himself... 'only today' I will let myself do my clinic a bit worse 'only today' I will not strive to listen, 'only today' I will dismiss the suffering of patients by responding with platitudes, 'just today'... But the 'only today' becomes routine. When laziness overcomes us it does not comply with only today, it always wants tomorrow. Then patients begin to wonder (and even to say), 'you are no longer the same as before'. When the professional accepts this, they accept nothing less than the loss of their self-esteem and from here slides inexorably into despair. If a hint of pride is left, it will motivate them to either seek other sources of intellectual compensation out of work, or they will divide their activity into 'routine' and 'research', in search of the area where they can say: 'Look what I am capable of doing, please, don't take everything else into account'. But 'everything else' tends to be what matters most to patients. Everything else, really... is what counts.
That is why the professional who has been in clinical practice for many years is united with the one who has just begun: both should look to the patient and the doctor-patient relationship with the fresh eyes of the beginner. As León Felipe tells us:
«That the things in the soul and the body do not scar so we never pray as the priest prays nor as the old comic says the verses. Not knowing the role, we will do them with respect...»
To these marvellous verses, Xavier Rubert de Ventós adds: we must overcome the inertia of habits (Rubert de Ventos X, 1996). There is a need to recapture the enjoyment of working and give the quality of adventure to everyday life.
This chapter will help us with this task. We will see, first of all, how we get an initial stereotype of the patient and the first frame of the clinical situation and how important is to be attentive to challenge this first stereotype and frame. We will also see some techniques to integrate patient data, mapping their demands and complaints, to allow the patient’s narrative during the first few minutes of the consultation, and to discover their way of making a gesture or a comment without importance. We will also learn to recognise when we are in emotional flow with the patient, what are the attitudes that separate us from this purpose and techniques to facilitate the patient’s narrative, all in a limited time frame.
Establishing a relationship: the impression the Doctor forms of the patient.
We said in Chapter 1 that three capital functions occur in the clinical interview (Cohen-Cole SA, 1991): We establish a relationship, we find out the profile of health and disease, and issue a series of information and tips. Let's see how we form a picture of the patient while listening too.
The image projected by the patient
We are very quick to label people. We do it by stereotyping, i.e. from one (or a few) salient traits, we guess if the person is honest, or the tasks which we could share. We need to do this to anticipate dangers, behaviours and opportunities. Since we were young we have allocated a part of our intelligence exclusively to do so. It is not something we are taught at school or university, but as a result of this intuitive thought our environment seems safer. We move aside from people whose reactions are unpredictable. Whilst simultaneously we strive to make ourselves predictable to others and we try to change our behaviour depending on their reactions.
We can only say ‘we know a person’ when we can more or less accurately predict their conduct. There is no real knowledge without predictive ability, that's what distinguishes mere speculation about a person’s behaviour from well-established knowledge. A technique to become more aware of another person’s character is to contrast the first impressions or quick judgments that form in our mind with what we can later confirm to be the reality. For example: "I think that this patient will be disorganised and will have difficulty taking medication correctly". Some predictions will be confirmed, but others will be refuted. The latter give us an opportunity to learn. Expertise is built on recognition of our mistakes. Here are some tips to guide us:
-
A person who acts decisively does not have to be intelligent or strong willed.
-
A very friendly person is not always a good friend. Warmth is a good business card which both good and bad people have learned to use.
-
A person we dislike can be an exceptional person, with great virtues that we aren’t aware of. And vice versa.
How do we go beyond the topics in this book, in our task of getting to know others? Adolescents are very polar with their perception of people: ‘I like/ I dislike’; they are expressions which do not accept intermediate positions. With age, we learn to be more even-handed and there comes a time in which we understand almost everyone, although there are people that elicit more of our sympathy than others. This natural evolution is positive, because it puts on hold negative stereotypes, and we give an opportunity to the patient to surprise us by contradicting the stereotype. One way to counter negative stereotypes that we form our head is to ask ourselves: ‘what if this person who I dislike, turns out to share something which is important to me or we share the a hobby which I love?’
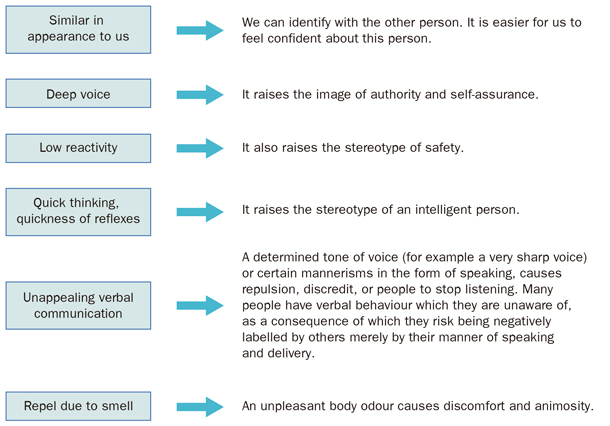
It is worth knowing the following corrections to errors of attribution (Borrell F, 2001 [Figure 2.1]).
In summary is it possible to, know people by stereotypes? Yes of course, it is impossible to break from them. We have a few boxes where we place people. The challenge consists, on the one hand, of counteracting negative stereotypes, the extreme judgments of black and white, and to expand the range of greys, and on the other hand, knowing the boxes which we use to place people in.
 |
|
Figure 2.1. Corrections to errors of attribution. |
Exploring part of the consultation: the semi-structured interview
For years we have been defending the view that health professionals should have a habit of work based on well learned tasks. We call this group of tasks a semi-structured interview, we summarise the exploratory part of this below.
-
Review the list of problems or the patient summary.
-
Cordial greeting.
-
Define the presenting complaint. The patient’s demands and map of complaints. Pathobiography.
-
Active listening ('vanishing point' of the interview).
-
Verify and complete data.
-
Summary of the information obtained.
-
Physical examination, if required.
In this chapter, we will address the first four points.
1. Before the patient comes to the room: review the list of problems or the patient’s clinical summary.
One of the great challenges of the clinical interview is to integrate the data we already have from the patient. The ideal would be to read the complete medical history before the patient comes into the room, but this is rarely possible. If this is not possible, the medical problem list, medications, investigations and the last consultation are the parts of the history that help us to become more oriented. We recommend the technique of open summary or open epicrisis (equivalent terms). It consists of a summary that is updated at each visit (especially when there are new additions), and must be readable in just a couple of minutes. It is the place where we explain about the patient: ‘since the patient became widowed, he is sad, his pain has become worse, he doesn’t have good adherence to his medication and his hypertension (HTN) is not well controlled’, which is different information from reading a list of problems such as 'hypertension, depression'. It does not exclude the list of problems, but it complements it which is advantageous. It is important that this summary includes phrases such as: ‘principal problem of this patient is...’, ‘must be controlled periodically...’, ‘in case of such a complication we suggest...’
An aphorism that we coined in the 1980s says: ‘an incomplete history remains incomplete until it reaches a Good Samaritan’ (Borrell F, 1988). Don't miss the opportunity to complete the basic data shown in Table 2.1. For data collection for a complete database, and a review by systems.
A particularly annoying situation is when a patient comes and stares to us. The doctor asks them: ‘how can I help you today?’ to which the patient responds with some displeasure: ‘You know!’ The doctor insists: ‘what do you want to ask me today?’ To which the patient responds, almost angry: ‘You told me to come today to review my blood results’. The case illustrates poor integration of data prior to the consultation.
|
Table 2.1. Database of medical history |
|
Family history and relationships. Job and hobbies. Past medical history, previous surgical interventions, drug history. Smoking habit, alcohol intake, use of recreational drugs. Physiological habits (urine, stools). Exercise. Diet quantitative and qualitative. Allergy to medicines and other types of allergy. Previous gynaecology and obstetric history. |
2. Cordial greeting
Do we have to shake hands with the patient? Shaking hands forces us look at their face and smile at each other. Only with that will we mitigate certain aggressive behaviours of the patient. On the other hand, it is important to mention the patient by name and smile. These are two basic markers of cordiality, which we studied in Chapter 1. Control your non verbal communication in the first few minutes of interview: ‘do I look tired?’ ‘Do I look distant?’ If you control your body language it controls your most intimate emotions.
Importance of the first minute
The symbolic value of the first minute of the interview is beyond doubt: it involves recognising the patient as the centre of the clinical act, not the papers or the computer screen. Avoid interference of any kind. For example, before answering the phone or checking the patient’s past medical history, we can say: "Please excuse me for a second". As simple as that. And writing? We recommend documenting the notes while the patient is undressing for physical examination, after this, or when the patient leaves. Writing a lot is not equivalent to higher quality, because there is the risk of information saturation and not being able to process the ‘truly important’.
Let’s look a little closer at this fascinating process of observation, listening and verbal and physical examination. How does an expert interviewer work? At the same time the interviewer strives to create a friendly atmosphere and watches carefully how the patient introduces himself. Details of the patient’s behaviour speak to the interviewer can convey certain meanings (Table 2.2).
|
Table 2.2. Everything about the patient speaks to us |
|
|
The way the patient comes into the room: |
|
|
Difficulty of the patient in opening the latch Direct gaze, smile Look at the ground, surrounds the chair Defiant gaze, furrowed brow Periorbital musculature laxity |
Suspect apraxia, which may be related to cognitive impairment co-operative Avoiding conduct, interest in delaying the onset Anger, extreme concern Sadness |
|
How the patient sits: |
|
|
On the edge of the chair Reclined Arms on the table (invading space) Crossed arms/legs Gesturing to get up Limp, hypotonic |
Discomfort, uncertainty and anxiety Indifference Security in him/herself, drawing attention from the clinician Defensive, uncomfortable Avoidance, wanting to finish Sad, depressed |
|
How the patient speaks: |
|
|
Attentively, synchronously Restless eyes, voice trembling, voice falsettos Sad eyes, final exhalation phrases, "disconnects" as if ruminating about what they are saying Clenched fist, jaw clenched |
Cooperative Anxiety
Sadness Anxiety, anger |
|
How the patient responds to questions |
|
|
Hesitantly, covering their mouth, repeated gestures Signs of anxiety, slight expressions of anger Mild cough, patient touches their neck, earlobe or nose |
Insecurity Displeasure Avoidance |
|
Modified Borrell F, 1989 |
|
Delineating the presenting complaint. Map of demands and complaints. Pathobiography
The difference between a demand and a complaint is the expectation that professional may or may not be the solution. For example:
Dr.: What brings you here?
P: To see if you could do something about the pain in my neck, because of the ringing in my ears I don't want to say anything.
Demand: 'solving the neck pain'. Complaint: ringing in the ears (the patient has no expectation of resolution). Sometimes it is appropriate at this point to make a map of all demands and complaints, as a global drawing can provide data for the diagnosis. Here's how the dialogue would continue if the professional had the purpose of making a map of complaints:
Dr.: Tell me, please, what other discomforts do you have?
P (a little puzzled): because right now don’t you know what to say...
Dr.: For example, how is the rest of your body?
P: Now that you ask, my arms and legs hurt... I have not been the same for the last two to three months. I feel quite tired.
Dr.: and how is your sleep at night time?
P: I sleep well at night, but then I feel tired all day.
Dr.: how is your mood at the moment?
P: Fine, it is fine. If it wasn't for this fatigue I feel, it would even be positive.
In general, an inexperienced interviewer tries to focus on a single reason for the consultation, and is even intolerant to people who provide various reasons for attending ('today I will address the neck and another day we'll assess the tiredness'). We suggest otherwise: we propose making a map of complaints and demands as complete as possible, because this is the only way to get to the bottom of the patient's problems. In the case exemplified above, note that the patient is drawing us an asthenic syndrome with multiple pains without any data that guide us to depression. Therefore, it is imperative to find out if there is also anorexia and weight loss, and other information that excludes a systemic illness. This orientation was not so obvious if we had focused exclusively on neck pain.
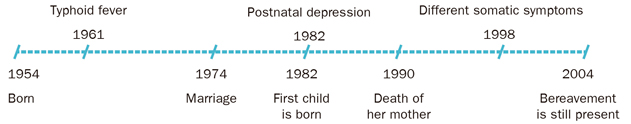
Pathobiography is another useful technique in confusing demands. We recommend it especially when the patient assumes that you have information that you don't actually have, or when you have started a possibly incorrect way of approach. For example:
Dr.: Your blood results are perfect.
P: So, I do not understand what is happening to me. Every day is getting worse and I am having more pain each day. Oh, and remember when I mentioned that my leg gives way? Sometimes in the morning I wake up and I fall because my leg does not support me. I told you this, but you ignored me.
At this point the doctor is confused because he has absolutely no recollection of the patient mentioning this topic. They may be tempted to settle the demand with a symptomatic prescription, but it would be a mistake. Later, when they mentally review what has happened, they would realise that the patient’s problem is poorly resolved. For this reason you may prefer to start from scratch, applying the pathobiography technique. So, he draws a line that is based on the patient’s date of birth patient and he reviews the chronology of all the patient’s medical problems, including the current illness. For example:
Dr.: Let's recap from the beginning. You were born in 1954; did you have a happy childhood? Did you have any major illnesses? When did you move to live in the city? How did you react to the birth of your first baby? Have you had similar symptoms previously? and now, when did you start feeling unwell? etc.
See Figure 2.2. This pathobiography includes the case of a woman who starts feeling depressed after giving birth to her first child, it deepens with the death of her mother and currently she presents with different somatic symptoms. When working out the meaning of the current illness, this data structured in a visual format will undoubtedly be very useful.
 |
|
Figure 2.2. Patient Eugenia B's pathobiography |
Exploring beyond the apparent presenting complaint
The reason the patient declares for consulting is not always what they really want to consult about. In Figure 2.3, observe the following decision of the clinical expert: 'I'm perplexed: the patient says they have come for X, but I doubt it'. The interviewer has reasonable doubts or is simply intuitive, so he puts the real reason for consultation on hold for some time. A clinician can take years to master the point of perplexity, because it is tantamount to admitting that 'I don't know the real reason for the consultation'. Know that we don't know. We fear not knowing because it is a form of weakness. But that is not the main difficulty. The main difficulty lies in continuing to work with a question mark rather than a certainty. Tell us: 'well, I don't know if this patient really comes to consult for his obesity, if he wants an emotional support or if he wants to take the day off, I don't know, but at the moment I'm going to work with the apparent demand'. Often new reasons for consultation appear at the end of the consultation (those reasons which really worry the patient), or specific demands which shed light on the whole process. In Table 2.3 we summarise some typical patterns.
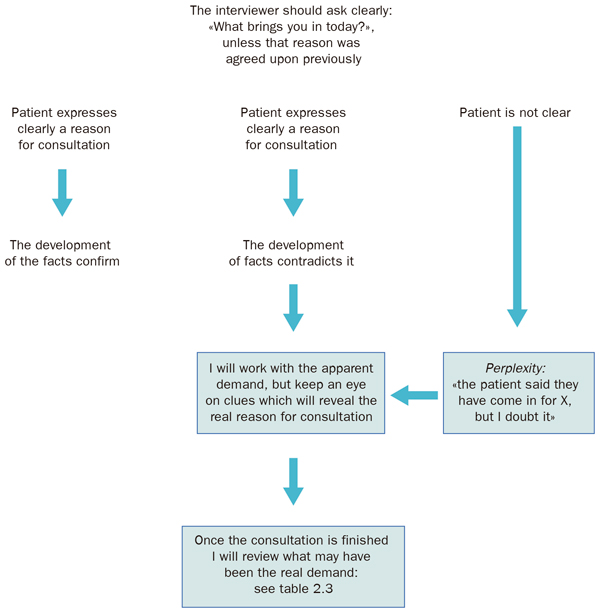 |
|
Figure 2.3. What brings the patient to the consultation? Working out our 'perplexity point'. |
It is of the utmost importance to predict, beyond appearances, the real reason that brings the patient today and in this way to the consultation, because this either a good or bad use of time arises. One aspect which distinguishes our model is that we affirm that there can't be good listening if the professional doesn’t know how to manage time or misuses the time available. If we unduly lengthen the consultation and people start to complain about the delay, the professional will be impatient, may not be empathetic and won't be in the necessary psychological position to listen creatively. Knowledge of Table 2.3, along with time management techniques, will give us the assertiveness point to tell us: ' it is worth letting the patient talk without stopping him, I'm doing my job well, and will recover this time later'.
|
Table 2.3. Beyond the apparent demand |
|
Some reasons for consultation which appears beyond the 'official presenting complaint of the consultation':
Business card: 'I introduce myself with this demand (business card), but in reality, I will soon reveal, I come for a different reason that may be dismissed by the professional if I mention it directly'. Rationality: the patient believes that some complaints are received by professionals better than others, for example those which are somatic in nature, anxiety or psychological distress.
Exploratory demand: 'I come with an apparent complaint of a cold, but what really concerns me is a genital lesion that has appeared. If the professional who sees me is the same sex and is understanding, I will tell them at the end of the consultation. Otherwise, I won't'; Rationality: there isn't enough trust, confidence or knowledge of the professional.
Shopping: 'First I have to get an orthopaedic product. Then, if the professional is friendly, I will add to the order: something for dry skin, a box of painkillers, etc'. Rationality: fear that the professional will refuse these requests; the interest of the patient is to take full advantage of the benefits.
I will make him feel sorry (or I am going to play the victim's card): 'I'll tell him everything that hurts me to get a very good consultation and so the Doctor realises that I am not acting. Then, I will ask for a medical report with everything he can include, so that I can be recognised as having a certain degree of disability'. Rationality: attracting the professional's attention and compassion the patient believes they will achieve certain benefits.
Pulling his ears: 'Today I will lengthen in the consultation regardless of how many people are waiting, so he understands that I need to be treated differently and when I ask for a prescription, this is something I need. I will only go faster if the professional does everything I ask for'. Rationality: the patient attempts to attract the professional’s sympathy and model the professional's behaviour, so that they yield to the patient's demands.
Heal the soul: 'Everything hurts, my head, arms and legs ... let's see if fixing these bit by bit you heal my soul, which is what hurts more'. Rationality: the patient experiences an emotional pain that increases other physical pains, or their emotional pain is expressed as a somatic pain. In any case, the patient vaguely requests relief for their emotional pain which hides behind their purely physical symptoms.
I only come to let off steam: 'I know that I won't be cured, nor do I pretend to think I will be healed, but at least you know everything I suffer. I have enough from the consultation just by talking, I don't want advice that will not help anything'. Rationality: the patient experiences some relief by simply speaking, sharing and even transferring some of their emotions to another person.
I saw him in the street : 'I saw him on the street the other day and told to myself “it's been a while since I have been to see the doctor” and that is true, because I guess it's time for my blood tests, isn't it?' Rationality: this item alludes to the iatrotropic effect (Feinstein A, 1967) (Yatros: medical; tropes: to), to explain why a patient attends today and not yesterday. There may be more acute symptoms, they may have heard a story on television that has scared them, may have seen us on the street, or another good reason to attend may have arisen. |
Active listening 'the interview leak point' and the technique of "pulling the thread”
Asking a lot of questions doesn't mean getting more information. Due to this, we insist that in the initial stages of the interview, space for the patient’s spontaneous narrative must be given, as shown in the example on the next page, where facilitations, interrogative sentences, reflective sentences and empathetic expressions are combined.
The example illustrates what we call 'emptying pre-made information’. Everybody coming to a consultation will have prepared some information; have a plan that more or less says, 'when I get to the consultation I will say this and that', and even sometimes (although this is less common) will plan that, 'I should not say such a thing because I do not want to reveal that ...’ However, in the ensuing dialogue the person may lower their resistance, and can even hear himself for the first time. These are the 'emotionally deaf', people who don't know how to listen to themselves or elaborate their own feelings (low insight), unless it is in an actual conversation.
|
EXAMPLE: «PULLING THE THREAD», ONLY A COUPLE OF LITRES OF COFFEE A DAY, Abbreviation: I: interviewer; P: patient. |
|
|
SKILL |
DIALOGUE |
|
Interviewer leaves it to the patient to establish the reason for consulting. |
P: I feel very tired. I: I see, could you tell me more about it? P: Well, for the last month I don’t feel hungry, I feel dizzy and I don't feel like doing anything. |
|
Facilitation |
I: Mmmmm... |
|
Words/Reflective sentences |
P: I've trying red Korean ginseng, but it didn't work. I: Not at all? P: Not at all. Because my neighbour said it could be depression, and that ginseng works well for depression. But I don't think this is depression. I: Why not? P: No, I think this is exhaustion... |
|
Empathy + cordial order |
I: I understand... go on, please. P: For the last months it's been crazy at work: I wake up at 5 am and I go to bed at 12 am. It’s really bad... |
|
Interrogative sentence |
I: I wonder how you've been able to cope with so much stress... P: I have coped by using with stimulants … |
|
Words/Reflective sentences |
I: Stimulants? P: Coffee, and something else… |
|
Facilitators |
I: Tell me more please... P: Not strong stuff like heroin, but some joints... |
|
Find and complete data |
I: Do you spend ... say ... 15 a day? P: No, how awful!... no, sometimes if I go to the pub in the evenings and someone invites me I get to ten, but it is rare. Usually it is about three or so. I: What other stimulants do you use? P: I don’t use cocaine, I took some several months ago but not since. I: Coca-cola or similar? P: Just coffee, but quite a lot. I: What do you mean by quite a lot? P: A couple of litres per day. I: Mmmm |
These people can literally discover that their relationship is not good at the moment while they are talking to us. These are floating feelings which become more concrete in the act of asserting them as real. When the patient says, 'I think there is no love in my marriage', they not only note the lack of love, but also they allow him to make it clear. In this act there is always a certain amount of commitment: commitment to tell the truth, and make decisions in accordance with this new reality. We must be consistent with what we say. Therefore a way of not making decisions is not talking about our feelings! But unfortunately floating feelings are around, bothering to exit in a dialogue and explain to the patient himself and surprised. Is it advantageous to have insight? We said that the person with insight is one that can recognise their feelings. In general they usually achieve this by simulating dialogues (virtual dialogues), in the privacy of their own thoughts, imagining that they are talking with significant others. To have insight we must lose our fear to face what we feel. This is precisely one of the causes of emotional deafness: lack of sincerity or cowardice with oneself.
In summary: in the first minutes of the interview, the interviewer may easily miss some comments from the patient which are true rough diamonds. Either you recognise them or they may not reappear.
Textual reading and suggested addition techniques
Another useful technique in the diverse clinic patients is the textual reading of symptoms. It consists of literally reading the patient’s expressions in an, almost shorthand way and then reading them a second time as if they were from an unknown patient. This technique minimises prejudice (and stereotyping) in relation to the patient which could block our reflective capacity. Moreover, when addressing somatising patients it is always useful to collect the literalness of their expressions, as the patient often forgets them and they think 'every time' that their symptoms are new and they panic. Reminding the patient that 'these symptoms' were similar 5 years ago (and reading their literal expressions) could be of great help.
Suggested addition technique (Coulehan JL, 1997) consists of suggesting to the patient something we think they want to say but they either don’t dare or can't find the words for it. This is a technique commonly used by projective interviewers:
Patient: I feel I don't know ... with a nuisance …
Interviewer: Here, where are you pointing? In the chest?
Patient: In the chest and it moves here, but it is not strong, but…
Interviewer: But it scares you?
Patient: It scares me because I think it could be my heart.
Interviewer: Could it be because you knew someone who had something similar?
Patient: Yes, of course, my father.
It is a technique that accelerates the interview and used well, can support communication flow, but it has the risk of suggested interpretations or questions with induced response for example, 'could it be that you also feel more nervous lately?' The range of possible responses is very limited.
Fourthly, the expert interviewer while listening to the patient has already drawn a mental picture of the person and their suffering. On the one hand, he has a basic interview plan (developing some general tasks, such as, for example, asking how, when and where the main symptom appeared), but simultaneously he asks himself 'how would I feel in such circumstances?'. It is empathic listening in which he imagines how he would feel with the patient's symptoms.
Framing and reframing the interview. Resistances.
'What is expected of me?' The answer we give to this question in every moment of the interview is the framing or intent of the interview . For example: a mother comes to an appointment with the practice nurse to get some advice about healthy eating; the interview seems to be agreed between the mother and the nurse. But at one point of the interview the mother departs from the script and starts crying. The nurse is first surprised, then irritated (there are many people waiting), but finally she guess that she is in a 'business card' type (table 2.3) interview and she asks herself: 'what is expected of me?' 'Right now, it is just to listen'. So she does and the patient tells her about a serious marriage problem. The nurse asks herself again: 'what is expected of me?' 'I don't think she is waiting for advice, she rather prefers to blow off steam'. However, the patient states: 'Do you think I should leave my husband?' Again the nurse has to reframe the interview: 'what is expected of me?' To give advice for which I don't have enough information, or the necessary psychological training to help. Therefore, I must make it clear to the patient that we can't leave the empathic listening frame. I am not prepared for a counselling type interview.
Something similar happens in this other sequence: a patient says: 'I have come for a sick note as I have horrible bronchitis'. 'What is expected of me?' the doctor asks himself: 'a sick note for acute bronchitis, however, I can see the patient has lost some weight... I have weighed the patient and I note involuntary weight loss. 'What is expected of me?', the patient will be happy with just a sick note, but my professionalism compels me to explore this weight loss further; I am going to suggest some blood tests'.
In this second case, note that reframing depends not only on the patient, but it also depends on what the practitioner considers good medical practice, which can change in each moment.
Behind a framing of the interview there is a forecast of actions required and an estimate of the effort that these actions will require (LR Beach, 1990). When a diabetic patient tells the nurse that his feet hurt, the nurse immediately projects an image of herself getting up from her chair, taking off the patient's shoes and socks, enduring the odour of the foot, etc. What will this effort yield? she asks herself. It is likely to have a high yield as undoubtedly he may have neuropathic pain because he is diabetic. In contrast, the same complaint in a healthy young patient can be dealt by putting his feet in salt water.
Therefore, to summarise, see below the types of resistances to reframing:
-
Resistance to physical effort: for example, resistance to get up from the chair (the common situation 'could you take my blood pressure'), or going to a home visit ('now that I should go and see that palliative care patient, it starts raining cats and dogs').
-
Resistance to cognitive effort: for example, resistance to consider a psychosocial diagnosis when we were following and a physical clue ('what if that dizziness could be depression?' No, it can't be because that would put me in a difficult spot. Ugh, go away laziness). We are afraid to think about depression in a patient who has lost their appetite 'what if other more important physical problems are missed'. We fear ourselves that by looking into the psychosocial aspects too much, we may end up missing the biological side. In other words: we don't trust ourselves. We know that a seductive hypothesis, which sheds some light on the case, paralyses other searches and hypotheses. To summarise: precisely because we do not control the reframing, we allow ourselves to be pinned down by the first hypotheses which are formed in our brain, the danger of this is that it expressly forbid us from thinking about psychosocial causes until we have discarded the physical causes. We term the psychosocial 'hop' when we move from an organic hypothesis to the psychosocial ones, and we recommend making this 'hop' an automatic habit.
-
Resistance to emotional stress: for example, when we make a diagnosis by saying... 'I'm sure you have such a thing', and the subsequent data doesn't point in the same direction. On such occasions, we compromise our self esteem. The more proud, arrogant or petulant the practitioner, the more they will insist on his first hypothesis, as if rejecting it will dent their pride. Even the fact that we advance a diagnosis before finishing the interview, makes denying it harder for us. Never make a diagnosis in a hasty manner, give yourself plenty of time.
Mistakes to avoid
Attitudinal errors
* «I know what happens to this patient»
«Looking at how the patient comes into the room, I almost know what happens.» This comment can have some truth in it (a good observer is able to guess many things), but it also tends to be the result of laziness. One thing is to imagine from our reality, what happens to the patient (what Bennett MJ [1998] calls sympathy by memory), but the other thing is to get closer to their world, their beliefs, expectations and their ways of interpreting health and disease (this is what is called empathetic effort). This requires an attitude of not pre judging what the patient is going to say to us, even if this respect does not equal neutrality. We can disagree or confront their beliefs, but we should always be oriented towards patient's benefit (rather than 'who is right').
* «I am just a technician»
“Patients cannot expect empathy or warmth from me. This is not a consultation with a Psychologist. I can give them my expertise, but I'm not here to be their 'mum or dad', and I can't fix their life. I understand diseases, not human happiness”.
We have noted this discourse between doctors and nurses in hospital and primary care, and even among some psychologists and psychiatrists. It goes further in some clinical departments and the practitioner uses the method of antipathy or coldness, to the extent that some of these comments can be heard: 'Look what has happened with somebody, hence his (bad) manners'. For this reason we say that the current problem in the health care relationship is not paternalism, but coldness of the practitioner. Moreover, the criticism of paternalism can be an alibi to justify this new style of being cold and distant. Note the following comment: ' I give the information I have to the patient so that they can decide what to do. But I don't go explore their feelings or let their suffering affect me'.
This comment shows fear of the other person, to prevent friendly relationships that can 'appear' in the health care relationships. This style, in the model proposed by Emanuel EJ (1999), would be an aseptic advisor. Here is a typical dialogue of an aseptic advisor:
Abbreviations: D: doctor; P: patient.
D: One possibility is to have surgery; another is to continue using stockings and postural measures.
P: what would you do?
D: It is you who has to decide. I've already informed you of the percentages of success and failure.
P: I will go for surgery.
D: OK, but keep in mind that these varicose veins will give you problems.
P: What would you do?
D: My opinion is irrelevant. You should decide.
P: OK, I’ll go for surgery...
D: Of course, but I am stating that this is your decision, not mine.
P: Then, I won’t have surgery
D: You'll see... then you will develop phlebitis and you will see how much you suffer...
In any human relationship, it is impossible to set aside emotions and feelings. Caring for the patient, said Peabody FW (1984), can only be made from true positive affection, that solidarity emotional quality that we have agreed to call empathy. We are not asked to give kisses or hugs, we are asked for an understanding look, a word of encouragement, we are asked for a minimum sympathy which shows our concern for the patient... or is the patient is not entitled to it? It sometimes happens that the practitioner is concerned, but has not learned to transfer this to the relationship. A professional concerned by a patient can appear distant or cynical. We come from a culture of modesty that makes it difficult for us to put our feelings on the table, especially when they are positive. However, doing so in a way which is honest, is an important step in building trust.
Whether we want to be or not, we are part of the influences that the patient wishes to receive. That’s why they come to see us to our clinic. We are also qualified like few others to give personalised advice, and even to take certain risks. Of course, the background tone will always be to be respectful of the patient's beliefs and decisions, but this does not preclude the fact that part of our job is to put the best decision (and the best of ourselves) at the service of our patients. In the example above:
P: What would you do?
D: We starting from the basics, firstly, you are who decides, because only you know the fear you have about surgery, and your work and family conditions, etc.
P: Yes, but...if I was a member of your family, what would you recommend?
D: In this case, I would recommend going for surgery, because the progression of your legs will be bad, and there is a risk almost certain of thrombophlebitis and other complications in the long run. There is also the surgical risk, of course, and the frequent risks include, those of general anaesthesia... (they are listed). From my point of view the balance between the risk of going for surgery or not going to is positive for surgery, if you assume that there is a general anaesthesia added.
P (after thinking about it): I think I won't have surgery. I would have to give things much more consideration before having an anaesthetic.
D: It is a decision which I respect. If you change your mind please do not hesitate to contact me.
* ' Arrogant ' attitude
The patients have to do what they are told. When they are caught red-handed straying from their diet or not taking their pills, it corresponds to scolding them. This attitude can be accepted by certain patients, but can generate a strong rejection in others. Scolding is one of the most constituent acts of a paternalistic relationship. But it may sometimes be necessary, as evidenced by the comments of some patients: '(practitioner) he became very serious and he rightly told me off for not taking the pills'. However to argue; emotional and pragmatic conditions must be fulfilled. When we get angry because a patient does 'what they please' we must calibrate the part of anger that corresponds to our sullied self-esteem and the part of anger which corresponds to the damage the patient has inflicted on himself. We can only argue with the patient for the second part, the first one must be neutralised. The pragmatic condition is that, additionally, if we argue because we believe that the argument will serve for something. Sometimes we are aware of that we reprimand without it having any effect on the patient, but we do it to unburden ourselves of responsibility ('I already said it').
A professional who argues a lot may have a guilt inflicting style. This style is often learned in the family background. When we have grown up in this environment, interpersonal relationships resemble a game of fencing, where each party takes 'advantage or disadvantage' on a score sheet with its 'credit and debits. Clearly part of every human relationship involves elements of 'giving and receiving', but we go wrong if that's what prevails. 'You must have done...' 'Where are we going if you don't take this seriously?' It matters little whether the professional is right or lacks reason, what matters is the climate it creates in the consultation. Should we therefore give up 'arguing' with patients? Not entirely, but when we do so, in general this should only be very rarely and we should do it for the patient’s benefit and not to fulfil our own emotional needs.
* Ignore our areas of irritability
Each professional has areas of irritability in their interpersonal skills. It is good that you know your own areas of irritability (Table 2.4).
|
Table 2.4. Trigger points that often irritate practitioners and how to transform them |
|
Patients who, at a certain point, say: 'and you, Miss, are really very young.' Internal dialogue that these patients promote: 'How absurd. Does not he realise that I am a doctor? He says this to annoy me.' Smart response: ' I will tell him with a smile and without sharpness: no, if I am a doctor/nurse, didn’t you know?'. |
|
Patients who request further investigations or specialist referrals, before we have been able to assess the problem. Internal dialogue that these patients promote: “Can’t they wait until I’ve worked out what the problem is first, the good Doctor that I am'. Smart response: 'Let's look at your problem first'. |
|
Patients who think we 'do nothing well'. Internal dialogue that these patients promote: 'If I’m doing things so badly, please change practitioner. Smart response: I will say, 'I realise that you are having a hard time at the moment' and I won't take it as a personal failure. |
|
Patients who are very talkative. Internal dialogue that these patients promote: what a selfish patient! He is not able to listen. Smart response: 'He must feel very lonely; I am going to listen to him for a while t try to relieve his loneliness'. |
|
Patients who won't leave the consultation room . Internal dialogue that these patients promote: But don't you see that I am tired and your time is over? Smart response: 'I will get up from the chair and guide him to the door in a polite way'. |
If we don't know our areas of irritability, we expose ourselves to a daily and persistent emotional drain. The skills of a clinician are built on a daily basis, and by no means as a runner on a 100 metre sprint. Everything that wears down the quality of our professional life must be analysed and reviewed and first and foremost our own negative emotions. Does this mean that we must not express our negative emotions? We can do it when:
-
We do this for the benefit of the patient and not as an outlet for our own emotional stress.
-
At the end of the interview, when we have already reached a therapeutic agreement or in any case when we've already figured out enough data to form an idea of the patient's problem.
A healthcare relationship presided by feelings of mutual collaboration is named 'being in emotional flow with the patient' (Goleman D, 1996). Here are some tricks to get into emotional flow:
Abbreviations: P: patient; D: doctor.
P: You always give me these tablets, but I what I need are x-rays.
D: I will take this into account. I always appreciate hearing what the patient believes is necessary to do. What about moving to the couch for a physical examination?
The practitioner has used a technique called intentional assignment. He does not give in immediately, but 'takes the information into account'. Only with this will be patient be relieved of some of their anxiety. Another patient comes in this way:
P: Oh no! The practice has changed doctors again! That's not very helpful, is it?
D (with a smile): I understand your anger (Renewal by objectives): However, as we are sitting here together now, I am going to ensure that your effort to come and see me is helpful. What can I do for you today?
In this case, the practitioner has implemented a renewal by objectives: moving the subject onto what the content of the interview should be.
In this case, the practitioner has implemented a renewal by objectives: moving to what the content of the interview should be. But do not confuse 'being in flow' with 'sucking up to somebody'. At times, fortunately only occasionally, the patient can be rude and crosses the border of what is acceptable. It is not easy to determine when this happens, because we are talking about patients with significant stress, or with cognitive impairment. A clear and malicious intention to damage our reputation or damage us repeatedly can draw the line, and make it convenient 'to distance ourselves from the patient' or even propose a change of practitioner. Here is a way of ending a professional relationship with a patient suggesting to the patient that they change to see another Doctor: ' I find very difficult to continue having you as patient in these circumstances... have you considered the possibility of changing to another practitioner?'.
Technical errors
We collect the Table 2.5 more frequent technical errors in the exploratory part of the interview:
|
Table 2.5. Technical errors in listening |
|
Non-existent or a very cold greeting. A lack of cordiality. Bringing in a reason for antagonism at the beginning of the interview. Not attentively listening to the phrases used by the patient at the time of coming into the consultation. They sometimes contain key elements which subsequently do not appear later on. Not clearly establishing the reason (or reasons!) for the visit. Assume it or accept vague explanations. Introducing elements of health education when we have not yet finished taking a full history. Premature reassurance. Not integrating the information obtained with the existing problems and diagnoses that we have in patient's medical history. |
* Non-existent or a very cold greeting. A lack of cordiality. Bringing in a reason for antagonism at the beginning of the interview
Example of lack of cordiality:
Abbreviations: P: patient; N: nurse.
P: I have this headache that I can’t live with! By the way, is there anything new for osteoarthritis? I'm in agony.
N: let's see, if we skip from one subject to another I can't clarify anything in my mind. Firstly, the headache, okay?
The right thing would have been:
N (sentence by repetition): You came for the headache, but it seems that your body is in pain. (Map of demands and complaints): Tell me all the body parts that hurt...
Example of premature antagonism:
P: I'm here as I need my repeat prescriptions. The pharmacist has already issued them in advance.
E: I don't do prescriptions in advance, in any case, I see patients.
The right thing would have been:
P: I'm here as I need my repeat prescriptions. The pharmacist has already issued them in advance.
E: Is there anything else you would like to ask me today?
P: No, just that.
N: This prescription is for an antibiotic, why are you taking it?
P: I have a urine infection. I know the symptoms and to not waste time I went directly to the pharmacist, I did well, didn't I?
N: What were the symptoms that you noticed?
After finishing the history taking and, if necessary, the examination, we will explain practice rules in relation to advance prescriptions by the pharmacist.
N: Indeed, it seems you have had a urine infection and that the treatment has been effective. You must complete 7 days of the treatment. On the other hand, our practice rules prevent us from doing advance antibiotic prescriptions by the pharmacist. This is due to there is a tendency to self-medicate with antibiotics in this area, and this can cause the medication to become less effective. For this reason we have received instructions from that once we have warned the patient, we can’t do any advance antibiotic prescriptions, because we always have an emergency service at your disposal 24 hours a day. As this is the first time you request it I will do this prescription, but please bear that in mind?
We understand by antagonism (Froelich RE, 1977, p. 29) that verbal or non-verbal conduct that opposes, criticises, blames or contests the conduct or the emotions of the patient. Its most common formulation is of blame: 'why didn't you do what I've told you?', 'if you don't lose weight I don't know why you come to see me', 'I don't know why I teach you gymnastics if you don't stop smoking', etc.
Blame is a more defensive than an aggressive weapon. A demand perceived as 'dangerous' (for example, a lady who comes in complaining: 'everything that I have told in order to get better, is not working'), it is deactivated with an attack ('how do you expect to get better if you don't follow the diet correctly?'). However, the advantage achieved by the practitioner occurs at the expense of creating tension. The deterioration in the clinical relationship affects an anti-placebo effect. The patient may wish that ‘what he has been told' doesn’t go well in order to return to 'protest', more vehemently.
Does this mean that we can' criticise patients? There is no doubt that sometimes a frank criticism (for example a criticism of a behaviour or a dangerous habit) should be considered as part of our responsibilities as 'carers'. In these circumstances we should observe some rules for constructive criticism:
-
Criticism must be made in an appropriate environment, without the patient thinking that we underestimate him or that 'we punish him'. From the beginning it should be made clear that it is constructive criticism with an operational purpose: improving his health through better collaboration.
-
Tone and voice, as well as vocabulary, should be the same standard as for any other health advice.
-
If we are tense inside due to the 'misconduct' of a patient, we might try to 'punish him' even without explicitly wanting to. The technique of self-disclosure (Duck S, 1981, p. 42; Headington BJ, 1979, pp. 64-72), which translates as ' showing / discovering our own feelings' and consists of telling the patient how we feel: 'I feel bad that you haven't taken everything we talked about the other day seriously', 'I take great a interest in your case, but I feel as if what we are talking about, you are not with me', etc. To some extent this is showing our fragility, but this point of fragility makes us more human in the eyes of the patient.
-
We must always leave the door open to the patient for an airy and positive output. Do not aim for an act of contrition!
*Not attentively listening to the phrases used by the patient at the time of coming into the consultation. They sometimes contain key elements which subsequently may not appear later on.
Example: 'I come because of this horrific dizziness and a buzzing sound in my ears. Oh, and I feel very anxious'.
The practitioner focuses on the dizziness and the tinnitus, when the key to properly resolving the interview was in 'I feel very anxious'. If the practitioner at some point in the interview just said: 'and this feeling of anxiety that you mentioned?’ it would have opened doors for knowing the psychosocial distress causing (or amplifying) the dizziness.
Beware! One of the most common misdiagnoses is the inability of the clinician to establish what we call double diagnosis. It consists of establishing as a cause of the patient's suffering due to not only a single cause in either the organic or psychosocial area, but two or more causes, either in the same area or in different areas. A double diagnosis would be:
-
Patient with reflux symptoms and epigastric pain due to: oesophagitis with hiatus hernia, duodenal ulcer, H. pylori positive, and anxiety due to stress at work.
-
Dizziness due to viral labyrinthitis which started 2 months ago and gets worse due to generalised anxiety disorder.
Actually a very high percentage of diagnoses should be double diagnosis, and, as shown, just think about any symptom felt by ourselves and different diagnostic categories we could apply. Are you known for being baffled? In this case, you are a greater risk of these types of misunderstandings:
* Not clearly establishing the reason (or reasons!) for the visit. Assume it or accept vague explanations.
Are you known for being baffled? If this is the case, you are a greater risk of this type of misunderstanding:
P (comes in complaining of a dental abscess that has slightly deformed her face): I come for this headache (pointing at the dental abscess when the doctor is looking at her medical records), that has scared me.
N (focusing too early): This headache, is it present in the mornings or in the evenings?
* Introducing elements of health education when we have not yet finished taking a full history. Premature reassurance.
Imagine a patient who comes with cold symptoms and the practitioner asks in the exploratory phase:
D: Do you still smoke?
P: Yes, I do.
D: So, if you continue smoking everything we could give you won't work. If you don't think about it seriously, we can't go anywhere.
The intervention itself may be correct, but try not to interrupt the exploratory part with tips or instructions (unless they are very specific). The exploratory part of the interview requires a climate of special partnership, and if we interrupt with advice we may make the patient become defensive.
Premature reassurances are a type of standard response: 'you will see how everything gets better'. It is almost a cliché to mitigate our own tension which we experience when a patient starts crying or tells us bad news. It is to prevent us getting involved in the subject and it is equivalent to an educated rejection, something we have learned in our social encounters (Bernstein L, rejection 1985, pp. 65 et seq.). When we meet an old friend and we ask: 'how are things going?’ we hope that his answer is going to be invariably: 'well, thank you'. To such an extent we meet this ritual is that a popular joke is that the person questioned answers: 'well, thank you, or do you want to hear the truth?'
What should we do when a patient tries to make us partake in their suffering? Here are some recommendations:
-
Find out the characteristics of the patient’s problem: 'what makes him feel this way?', 'how is the partner taking this situation?', 'what plans does he have to improve the situation?', 'how does he think I can help him?' etc.’ If you don't have time to do so, or the consultation was already finishing, you could rehearse: 'do you think we should see each other again with a bit more time to discuss this problem further?'.
-
Some health problems have few solutions, for example: irreversible blindness, chronic illness, etc. But even in these cases, all problems have two aspects: a) the problem itself, and the possibilities of improving it, and b) the way in which the patient can cope with it, and adapt their life to it. Don't be influenced by the patient's pessimism, but on the other hand, ask yourself: how would a person with an optimistic frame of mind react in the same predicament? Even in the worst case scenario, a supportive empathy will always be possible (and no 'assurances'), and can be expressed with a glance or a gesture (Tizon J, 1982, 1988).
* Not integrating the information obtained with the remaining problems and diagnoses that we have in patient's medical history.
The patient tells us some symptoms they have as if they are new, but they have actually already reported them a few months or years ago. But the worst case is that the practitioner doesn't realise this and duplicates investigations. This would be avoided if we were able to integrate the data from the clinical history (remember the open epicrisis method)
Situations gallery
We will see in this section:
-
When listening hurts
-
The patient with multiple complaints
-
The intruding relative
-
When the doctor and the patient speak different languages
When listening hurts
In the first example, the practitioner attends the carer of a terminally ill patient. The process stretches and ambivalent emotions appear.
Example: a carer on the verge of giving up.
/1/Family member: It is an unbearable situation. I'm about to explode.
/2/Nurse: You have to hold on. You will have time to cry later, but now you have to hold on a little more.
/3/Family member: I feel very unwell because I can't do anything, I can’t keep her well, and I can’t bear to see her in so much pain until she dies.
/4/Nurse: You don't have to think about death. Your mother can still live. While there is life there is hope.
Comments
1. What are the successes and errors in this brief conversation?
In /2/ the nurse says at the beginning: 'You have to hold on. You will have time to cry later, but now you have to hold on a little more'. This intervention can't be considered wrong, if done with enough empathy. Interestingly, the opposite intervention can also be correct, namely: 'you are doing well in expressing your feelings. If you have to explode, explode; cry or shout if you want to. You have every right in the world, because you are dealing with a lot’. What determines whether to use one approach or the other? One is suitable for carers who have the facility to cry (and even do so frequently), and their problem is rather to have the courage to face the hardships. The other one is for carers who are very contained.
In /4/ nurse said: 'You don't have to think about death. Your mother can still live. While there is life there is hope'. Here we can say that mistakes have been made. It is useless denying death and giving false hopes, particularly when the carer is trying to adopt a realistic position. When the practitioner has not assimilated that the patient is dying, when he is afraid, they may reinforce attitudes of denial by repeating typical social frames. From this arises containment capacity as a way to hear what the patient says which does not necessarily lead to giving advice ('you should...'), or an action. To have containment, we must distinguish between my way of being from the patient’s way of being. Containment gives a quality of quiet listening. It must also be clear that we do not always need to give advice indeed advice may also have its own iatrogenic effect.
2. Should we disagree with the carer because she indirectly expresses that she wants her mother to die?
Quite the opposite. It is normal to carers be torn between their affection for the person and the pain they experience by seeing the person suffer. You cannot avoid thinking about the relief that they will experience when the patient dies, and that arouses feelings of guilt. The practitioner can normalise and legitimise their feelings: 'it is very normal in your situation wishing it all to end, because it is very painful to see a loved one suffering so much; A lot of people in a similar situation to you feel like this’.
What should we do in such situations?
In these cases the most important thing is our manner in front of the patient rather than the words we use. It should be warm, close, comprehensive and, above all, calm. If the practitioner is behind a desk, they should move their chair next to the family member. Here is a dialogue demonstrating the interviewer legitimising and normalising the ambivalent emotions of the carer:
/1/Family member: It is an unbearable situation. I'm about to explode.
/2/Nurse (empathises, pausing briefly to give the interview a slow pace): You have taken on too much responsibility and work at home for quite some time.
/3/Family member: I want to cry, I want to shout, but I can't...
/4/Nurse (enables and supports emotions): Even if it’s only to say what you’ve just said, it is good for you, as you are venting a little ...
/5/ Family member: Sometimes I feel I am a bad person because I would like it all to end, and that they will no longer suffer.
/6/Nurse (legitimises): When you love someone and you see them suffer, you have every right to say that your emotions are stretched
/7/Family member: But I have no right to think about his death.
/8/Nurse (legitimises): These are very normal thoughts, especially when the burden of the whole situation falls upon you.
/9/ Family member (sobbing): He has always been very good to me, and I now think that it would be better if he was dead.
/10/Nurse (offering a tissue, drawing importance to the emotional ambivalence): What counts is not what you think, but what you are doing. (Increases self-esteem): Your role has also been essential. If it had not been for you, he would have been admitted to hospital and he probably wouldn’t have been as well looked after as at home. Not that you should have any doubt about that.
|
Remember, situations when listen hurts:
|
The patient with multiple complaints
Patients attend health services an average of six times a year. However, 20% of patients consume 60% of our material resources (time, medication and investigations). The current trend is to consider that all of them have good reasons to do so, and that, in any case, the challenge to lower their frequent attendance and multiple complaints, falls upon the health team. Note this first scene:
Example: The patient with multiple complaints
Abbreviations: P: patient; Dr.: doctor.
P (taking out a list): Doctor, today I’ve brought you a written list, because I always forget things.
Dr. (with a tired tone): I don't know if we will have time for so many things madam...
P: I feel very poorly, you will see Doctor, I can't continue like this...
Dr. (showing signs of impatience): Let's see, what can I do for you today?
P: Firstly, I have the issue about my kidney stones. I am taking calcium and I think that if I have kidney stones, calcium is not very good for them, is it?
Dr.: Of course it is alright, there isn't a problem with it.
P: But I've heard that...
Dr. (impatiently): It doesn't matter what you have heard, because I’ve told you there isn't a problem. Let's move onto another problem on the list.
P (grumbling): Ok, well, I have a cough, but I already feel a bit better... (suddenly changing tone of voice to another more cheerful one) Oh, by the way, doctor, I'm sorry, but today you will have to look at my bum.
Dr. (somewhat perplexed): why is that?
P (cheerful): Because I have piles like never before.
(Doctor proceeds to do a rectal examination. Returning from the examination couch)...
P (with the list in hand): Wait, doctor, I have several other things, I say this because if I sit down then I will feel too tired to get up again.
Dr. (puzzled): Well, we have looked at two points of the list today, we could look to another two points another day.
P (desperate): but the main reason I was coming today was about this dizziness and because the pharmacist has found my blood pressure to be 210!
Comments
-
Is 'one presenting complaint per visit' correct?This aphorism of 'one problem per appointment' leads to the patient's frustration and doesn't allow the doctor to get to the bottom of the problem. Consultations are multiplied in a climate of insufficient understanding and are less effective. As we said previously, the practitioner should make a map of complaints and demands, because this bigger picture of the patient will help him, to understand the patient to a greater extent.
Well, once we have defined that there are 'several problems' which we are asked to address, we will proceed by addressing each one in sequential order to its resolution. We will open an episode of disease for each of them (provided that you understand that they are separate issues), and if we don't have enough time to address them at the appointment, we will offer the patient a further appointment.
-
What is the main mistake of the practitioner?The main error is the tired and irritable emotional tone he shows. The patient feels vulnerable and their pessimism is reinforced. This leads them to arrange another appointment soon to clarify many of the points on their 'list' which remain unclear. The emotionally proactive practitioner (Borrell F, 2002) remains calm and even injects optimism into the relationship: 'I see you look very well, Sarah' 'congratulations on these blood results, they have come back as if you were 20 years old'. This type of phrase, when said by a 'super scientist' practitioner, connects with the symbolic world of the patient and may change their perception of their well-being. This should always be done on the condition of not lying, not even if well intentioned. Don't forget that often being healthy is not as important for our personal happiness as believing we are healthy.
-
Is there any significance to the way in which the patient introduces her requirements, and in particular the request for a rectal examination?In general, patients give us an 'agenda' and a few pre-write what they wish to be the content of the visit. The order and meaning of these demands should not go unnoticed. The patient has scheduled a longer visit than the doctor is willing to grant. For her it is a ritual in which there is an important social component. She wants to 'be able to explain' and possibly in her mind she has imagined a gentle and loving conversation with her doctor. This pattern is typical of lonely patients, in which a visit to the doctor or nurse is a form of socialising. The change in tone with which she announces her request for a rectal examination may be to mitigate her modesty, or could be to accommodate some erotic tension. Both possibilities should be taken into account, since in communication, it is always preferable to consider several hypotheses, simultaneously in a flexible manner, rather than a single one.
-
When the patient comes back after the rectal examination she introduces what appears to be her main concern... How should her doctor proceed?
First, the doctor must detect their own emotional reaction; undoubtedly this is not to re-open the interview. They should also assess the implications if what the patient says is true. It is precisely in situations like these where a good deal of flexibility marks the difference between committing to ones initial reaction and avoiding a clinical error. Measuring her blood pressure will take just a few minutes. Not doing so, on the other hand, may activate later anxiety: 'and if indeed what if she has a hypertensive crisis?' The personal cost of this anxiety is equivalent to a thousand times the small effort of taking her blood pressure.
¿What must we do in such situations?
-
Ask the patient to read the entire ‘shopping list'. Especially before asking the patient to get off the examination couch ask: 'are you sure we should not look at anything else?' If despite this, the patient pulls out another new request at the end of the interview (a request that doesn't make us anticipate any serious or imminent danger to the patient), we will suggest quite frankly: 'well, if this is ok with you, we will leave this issue for another appointment’. If the patient insists, we will clarify: 'unfortunately I don't have more time for you today'. It is very difficult to address more than... (i.e. the number of presenting complaints addressed here) problems in a single visit, so the best thing would be to arrange a follow up appointment with me for …'.
-
Differentiate the 'new' from the 'old'. These patients are at a high risk of clinical errors, basically because the professional applies the rule 'you come to see me about so much that I disregard you'. Another doctor or nurse who evaluates the patient without prior knowledge of them can discover disorders and diseases with a possible therapeutic approach towards them. Reconsidering these patients 'as if we didn't know them' tends to have a positive impact on the prevention of errors.
-
Try to regulate the frequency of patients’ visits yourself, and that both the medical and nurse appointments fall on the same day. Gradually reduce from weekly visits to fortnightly and from fortnightly to monthly. Use the phrase: ' I would like to see you in... days'. When the patient requests an earlier appointment without a compelling reason, don't refuse to see them, but then agree an interval until the next appointment which is acceptable to the patient.
-
Try to encourage elderly patients with cognitive impairment who come to see you very frequently, to attend with a family member or carer. Refer these patients to social services so that they can evaluate the patient’s need for support, aids at home, etc. Sometimes their visit reveals this deficit (which, incidentally, will never be revealed with a consultation).
Let's see these principles applied in the previous interview:
P (taking out a list): Doctor, today I’ve brought you a written list, because I always forget things.
Dr. (with a cordial tone): I welcome it. It is very good that you have come well organised. If you will allow me, we can read the list together.
(Both read all points of the list.)
Dr.: You have brought me 10 points, but hopefully, in the time we have today, we can deal with a couple or three of them... which ones do you think are the most important?
P: Doctor, all of them are important!
Dr.: Because of this I will arrange another appointment to see you next week, and we can address the rest then. Which point is considered the most important today?
Once two or three have been prioritised, the practitioner moves to solve them. The strategy of 'negotiating the demands in instalments', which we stand by here, does not contradict the map of complaints and demands outlined above. Although we postpone requests, the doctor has to have a full map of complaints, this is the only way to obtain good diagnoses. Imagine how hard it is to diagnose a patient with depression if we fractionate all the symptoms they have! For example, if at the end of the interview the patient adds:
P: oh! And my back! Aren’t you going to look at my back?
Dr.: Of course I will. Your back deserves a full visit. I would like to see you in 10 days, look I am going to book it myself, although I am very busy, for the day... We will assess your back and address two more points from your list. Is this day ok with you?
|
Remember, with a patient with multiple complaints:
|
The intruding relative
A strong biomedical tradition has demonised the relative, who by definition 'we need to silence' so the voice of the ‘real patient' can rise. This is a serious mistake which has led us to underuse a huge potential both establishing the symptoms and as a therapeutic ally. We are not we going to deny that the presence of a relative can sometimes be uncomfortable. See, for example, the following situation:
Dr.: How can I help you today?
John: I have a cold again.
John's wife: This is not correct, doctor. It is not a cold; it is bronchitis because he doesn't stop smoking. He ignores what you said. You have to scare him because otherwise I don't know when he is going to stop.
Dr.: Tell me more John...
John's wife: He spends all night coughing and because of it, I am not getting any sleep.
Dr.: Did you have a fever John?
John's wife: No fever, but the other day going up the stairs he got very pale, explain everything to him John! And he also had a pain here (pointing his chest). Come on John tell him everything! You shouldn't hide anything from the doctor. It would go against you if you don’t tell him everything, as he can’t help you properly if he doesn’t know everything.
Dr. (irritated): Madam, but don't you see that you have overwhelmed him, so there is no way he can say anything as he can’t get a word in?
Comment:
1. Do you notice any errors in the way the practitioner acts?
The last sentence from the doctor is undoubtedly sharp. He makes a judgement about the couple's relationship ('you have overwhelmed him'), and he gives free rein to his impatience.
2. Are there any key symptoms which were important in the previous dialogue?
Several key symptoms have appeared:
- The patient says he has a cold, he has cough but does not seem to have a fever (this point should be confirmed), and he is a smoker.
- Furthermore, it appears that the patient has had an episode of chest pain, perhaps associated with vasovagal symptoms.
- Finally, the interpersonal relationship of the couple is a useful data, as we will see below.
3. Can we deduce something about the relationship of couples who present in this way during the consultation?
The way a couple interacts is due to a relationship previously established and consolidated over the years. The practitioner will quickly realise who is in control of the situation, the degree of mutual dependence, the degree of appreciation and respect between them, etc.
In the case we are dealing with:
- Neither member of the couple could be so intrusive without the passivity, or concession, or secret interest, from the other member, to act in this regard.
- When we meet with a member of the couple who acts in a very intrusive way, we need to ask ourselves a differential diagnosis which encompasses various situations: a) the relative is detecting a risky situation and the member with better social skills takes the initiative; b) one member of the couple (who is also the dominant), is irritated with the other member, and makes them feel uncomfortable by expressing symptoms which either blame him, or more commonly, which annoy her; for example: 'he snores and doesn't let me sleep'; c) The communication pattern is due to a type of dependency accepted by the other party. This sets up the pattern of their interpersonal relationship and it has been established for some time, and d) there are sadomasochistic aspects (for example, verbal insults or psychological abuse), and the dominant member wants to avoid the patient saying inconvenient things, for example things which may reveal physical or psychological abuse. In such cases, we can get the patient to attend another consultation with the excuse of needing to perform a procedure. Sometimes a mother wants to reveal information about her child which her child is not aware she knows (for example, that they take drugs). If we have this suspicion, we will ask more specific questions (do you use cocaine? and ecstasy? etc.), following the aphorism: 'the patient may try to hide things, but almost never lies'.
What must we do in such situations?
-
Apply a technique we call 'emptying interference' (table 1.1, Chapter 1): go to the invasive relative with cordiality and invite her to say everything she has to say. Take the information provided to you seriously.
-
Ask the patient to unreservedly express the reason for consultation, for example: 'And in your view, what brings you here today?' Confirm the most important parts that the relative has provided: 'what do you think about what your wife has said in relation to...? This is what we call 'the bridge technique'.
-
When a relative keeps on interrupting and you do not consider their contributions useful, propose an intervention agreement: 'well, you have had some time to tell me everything you wanted to, what you think if we now leave this time to xx?’ If despite this the relative insists on speaking, we could take the patient to the examination couch and continue the history taking there, whilst performing the physical examination. If the relative still invades the patient's space, it may be appropriate to take the patient to another room, or ask the relative to leave the consultation room (creation of a new environment): 'Please cold you leave the room for a moment? You can come back in shortly'. Try to do it with cordiality.
In the analysed case:
Dr: How can I help you today?
John: I have a cold again doctor.
John's wife: This is not correct, doctor. It is not a cold, it is bronchitis because he doesn't stop smoking. He ignores what you said. You have to scare him because otherwise I don't know when he is going to stop.
Dr (asking the patient for his consent to do an 'emptying interference'): What do you think John, if we let your wife tell me everything she wants first, and then you also tell me all you want to?
John's wife (without waiting for her husband's consent): Well doctor, apart from that he ignores everything you said, you have to scare him because he won't stop smoking. The other day I was very scared, because when he was climbing the stairs he became pale and had pain in an important part of his body (pointing the left side of her chest).
Dr: Do you want to say anything else about your husband?
John's wife: No, not about my husband. But I have also come in with a pain in my shoulder.
Dr (ignoring the demand from the relative): If this is ok with you, now we are going to move onto your husband, is this ok? Let's see, John, you came with a cold, didn't you?
P: Yes, I did
Dr (bridge technique): And what about the pain when you were going up the stairs which your wife has told me about?
On the practitioner's agenda the priority appears to be to clarify these symptoms which could indicate an angina type of pain, even if the patient denies or undervalues it! As we said above: avoid dependence on field. Professional goals do not have to agree with the patient's (or relative’s) goals. The patient's goals have to be taken into account, but you also need to incorporate the other objectives which are derived from your clinical knowledge.
|
Remember, in the face of an intrusive relative:
|
When the doctor and patient speak different languages
Aisha, who is 32 years old, attends with her daughter Anaya who is 10 years old. Both are African. Anaya speaks English quite well, but her mother doesn’t.
Abbreviation: N: nurse.
Anaya: My mum says she has tummy ache.
Aisha points to her epigastrium are while the girl talks
N: Please could you ask her how long has this been going on?
Anaya: For quite a few days
N: Please could you ask her whether she has abdominal cramps?
Anaya: I don't understand...
N: Please could you ask her whether she has diarrhoea?
Anaya: She says she has in front
N: Please could you ask her whether she has a burning sensation when passing urine?
Anaya: She says she has.
N: Please ask your mother if she can go to the toilet, and do a urine sample in this little bottle and bring it back to me.
Urine dipstick is positive for leucocytes, so an antibiotic is prescribed for a presumed urinary tract infection. The following day the patient is admitted from the Accident and Emergency department and she has emergency surgery for an ectopic pregnancy.
Comments
1 What was the main barrier to establishing effective communication?
The main barrier was the laziness of the interviewer. He thought that he could save himself having to perform a physical examination based on the history from the girl, and the alleged dysuria. In this case the need an examination of abdomen and pelvis, was inescapable due to the blatant gestures of women indicating lower abdominal pain. The value of the word was secondary.
2 In the absence of a translator, should we deny assistance to this type of patient in order to prevent clinical errors?
We should never deny assistance. There is a telephone to be able to do simultaneous translation for most languages. If this is not possible, it is best trying to deal directly with the patient, and use the child occasionally for specific words. Finally, we should always compensate the lack of oral communication with a thorough physical examination, while still communicating on a non-verbal level as we examine the patient. If doubts persist about the diagnostic orientation, and answers to relevant questions are required, we will proceed to ask for a translator, or we will refer the patient to a centre where one can be provided.
What should we do in such situations?
-
Try to have at your disposal a 'book of reference (in different languages containing drawings with illustrative phrases of the most common problems).
-
Familiarise yourself with the use of telephone interpretation services, or failing that, with volunteer services which offer a similar function.
-
Agrees with the patient a non-verbal simple code: 'here yes/no pain', 'do what I'm doing', etc.
-
Even if a family member or friend translates for the patient, do not forget that they may make significant errors. Don't forget to perform a thorough physical examination and give independent weighting to the examination findings from the history data.
-
In certain situations when a relative acts as a translator, they can become confused and respond as if they were the patient. Try to assess whether the relative is a skilled translator: they use a similar length of sentence to the patient, they address the patient each time, and they strive to be understood...
Advanced concepts
Types and purposes of listening
The listening we practice in our social relations is an operational listening, directed to solve everyday problems. When we get into more intimate conversations we listen, in part, out of courtesy, to accompany the other person and, if there is friendship, partly out of sympathy, to influence each other's emotions or opinions (sharing our intimate reality is colouring the world in a similar way).
Professional listening is different. On one hand, sympathy is replaced with empathy. The concept of empathy enables the clinician to understand in a warm way without being emotional. This allows us to go beyond the superficial contents. A clinician not only notes what the patient says, but how they say it. A 'difficult' patient may have a cognitive impairment, sudden euphoria may make you suspect hypomania due to antidepressant intake, digestive symptoms mentioned 'incidentally’ by the patient make you think of ulcerous dyspepsia. This is semiological listening: moving from an anecdote to a category of illness.
Sometimes a descriptive listening has occurred as opposed to a semiological listening (Fernández Liria, 2003). The advice would be more or less: 'it is better that you listen in a non judgmental way to what the patient says in every moment, allowing, but not causing, a scenario of what may happen to them to form in your mind'. This strategy would make it possible to pick up nuances of reality which are impossible to perceive when we are listening for the sole purpose of 'labelling'. Something similar happens when we try to pick up literally the more typical phrases of the patient in the clinical history, or what we previously called textual reading of symptoms. However, after a first half where we are sponges absorbing information, there must be a second half where we interpret the information. Not everybody obtains the same interpretation of the information absorbed. The semiologic attitude is characterised by:
- A view of the patient that separates what we think or feel about them from what we think and feel about the symptoms they present with. For this reason one is a bad doctor for their best friends, because we don't dare to think 'the worst'.
- A gallery of images and situations of reference. They are the code-source port of call where we go to compare everyday situations with the images. To obtain the maximum benefit, the clinician should refresh their skills on a regular basis (for example, through studying of clinical cases, refreshing their memory with typical images, etc.)
- The willingness to think creatively about the patient. Go beyond the first labels. Create from reality new code-sources to enrich our vision of the world.
Let's imagine that the patient says:
- 'I fight with everybody. I am very nervous."
Instead of thinking: 'what a madman', the clinician says to himself: 'aggressiveness and nervousness, we will seek more data on the psychosocial aspects'.
Semiologic listening must be performed not only on what the patient says verbally, but also on what their body language and their facial expressions tell us. This means the clinician must be alert and concentrating to develop the information spoken by the patient into facts with clinical value. For example:
- 'This patient says he doesn't leave his house to go shopping because he gets dizzy. I can see he looks nervous and anxious... It seems unlikely that his dizziness originates from a problem with his ear, but he seems upset when I address his mood'.
One of the great difficulties of semiologic listening is practising it when: a) we give little credit to the patient, or b) we consider the patient as a citizen and very little as a patient. As an example, see Table 2.6.
We find semiological data only when our intelligence withdraws from the mechanical aspects of obtaining good data, and focuses entirely on interpretation of the data. This is very difficult or impossible to perform when we have emotions, especially negative emotions which interfere with our ability to listen.
|
Table 2.6 The danger of not believing the patient
A patient comes in requesting a sick note for generalised weakness. The doctor thinks: 'here's another patient wanting to claim sickness benefit. This classification removes the value of the patient to give him the value of ‘seeking sickness benefit', and consequently he already does not practice semiological listening. The patient complains of diffuse weakness 'my legs hurt and I can't work like this'. The doctor reluctantly explores the patient’s history and can't find anything relevant. There is a discussion on sick leave, and the doctor loses an excellent opportunity to diagnose Hodgkin’s disease which would only have been evident by performing a chest x-ray. |
Listening and emotions
It was probably Karl Rogers (1980) and a little later the school of Palo Alto, who began using the term empathy. Almost everyone believes that it is an old word, because of the speed with which it became popular, but it is actually a modern intellectual creation, largely collective (like all important words) and certainly very refined.
Empathy is, firstly, an emotional state of the interviewer that allows them to detect emotions in the interviewee (first moment of empathy). Thanks to this they can show the interviewee that an emotion has been noticed (second moment of empathy), whether it is done in a verbal manner (solidarity expressions such as 'I see', I can see your suffering', etc.) or in a non-verbal manner (equivalent facial gestures). A smile can have an effect of cordiality and in another context an empathetic value. The most common empathetic statement would be: 'I can understand how you feel'. In empathy, the non-verbal component outweighs the verbal one. An empathic sentence such as 'I can see you are not having a good time' pronounced with disdain or fatigue, has an effect opposite to the desired effect: it would be perceived as a criticism or antagonism. Do not confuse empathic interventions with value judgments ('you did what you could'), or with premature reassurance ('everything is going to be fine').
Empathy differs from sympathy due to the quality of solidarity associated with sympathy. Sympathy asks for a unique and total willingness towards the relative or friend, to attune with them and participate in the manifestation of their emotions. Empathy, on the other hand, permits us to put ourselves in other people shoes and feel their pain, with the mind more than with the heart. We empathise when (for example, by telling them in either a verbal or non-verbal manner: 'I can see you are suffering'), we offer ourselves as a possible support and an opportunity to help, but unlike the sympathy of friendship, empathy is an attitude governed by standards of professionalism. Empathy comes from the following assumptions: a) it is not necessary to be suffer with the patient, just realise that and recognise it; b) A little hypocrisy is permissible, or the 'theatre' of declaring that we 'feel' someone's pain when in reality we do not as the consequence is positive not only for the patient, but for the professional too (we can become as used to the emotional warmth and solidarity, as the actor who ends up believing his role); c) you have not only the right but also a duty to keep an emotional distance from the patient, because this therapeutic distance allows you to think and decide in an analytical and unbiased way. It is a medical or nursing friendship (Laín Entralgo, 1964) from which we can argue 'no': 'I can't do what you are asking me because...'. See other features of empathy in Table 2.7.
|
Table 2.7. Differences between warmth, empathy and sympathy |
|||
|
|
Warmth |
Empathy |
Sympathy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
However, while the concept of empathy is very clear, practicing empathy is complex. We come from a culture of modesty where the external manifestations of solidarity are almost taken as an overflow of affection. Professional empathy asks exactly the opposite (Figure 2.4): staging a solidarity gesture when we have very little affection for the patient. Isn't that 'acting'? a student asks rightly. Yes, it is, to a certain extent, it is. But acting is not hypocrisy. Let's say it is a staging that repeating it creates a habit of solidarity in us. This is the rationale and the ethical basis.
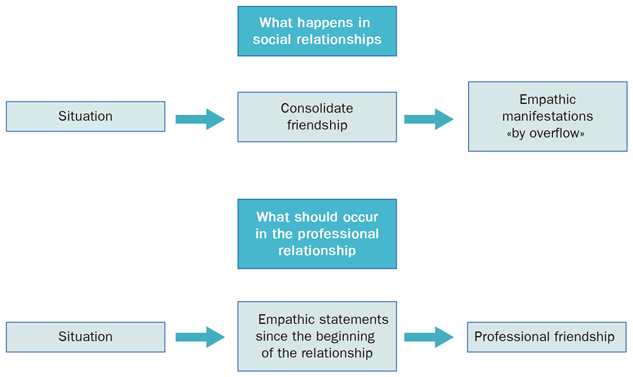 |
|
Figure 2.4. Difference between empathic manifestations in a social environment and in a professional environment. |
When we talk about empathy we can't fail to reflect on our patience. It is not possible to have positive emotions toward the patient without a good dose of patience. Can you imagine trying to make an empathic statement when feeling irritated or in a rush? For some people, patience is equivalent to knowing how to suffer (Sadaba J, 1999). We prefer to define it as the emotional quality that we accept what is inevitable as inevitable (Platt F, 2000). It is inevitable that an elderly man of 85 years of age will take time to move to the examination couch and undress. Patience is to allow the present flow without pushing it and not suffering for not being able to go faster. A woman who experiences domestic violence will take time to open up about it, and will welcome the time when she manages to do so. Sometimes we have to heal ourselves of the desire to heal, but not the desire to understand (Guillem Salvador, 2002). With patience, we get to the rhythm of things, and this in itself is already empathetic. Have you considered that a contemplative quality can fit into the consultation? When one achieves this quality, patience ceases to be a suffering in order to become in tune with the patient: we tune into the rhythm of the inevitable.
Good communication versus poor communication
There are two basic positions in any human relationship to Suchmann (1998): collaborative or competitive. In the consultation we take for granted that we are in the first position, but the truth is that there are loopholes for suspicion, ridicule, hostility, resentment, humiliation or blame, among other negative feelings.
The most natural emotional style is what we previously called reactive: pleasant with people who behave in a pleasant way with us; hostile to those who are hostile. To each we paid in kind. The opposite of the reactive style is the proactive style. With the proactive style we try to break the vicious circle of negative emotions. Some people seem to always be happy and optimistic no matter what. They are proactive people in all facets of their lives. Their ability to permeate the environment they are in with these qualities makes them highly prized. We can learn a lot from them, we can for example learn a sense of humour: to smile and laugh with the patient, but never at the expense of the patient. We can also learn the uselessness of resentment. Resentment is a fantasy of vengeance which has never been carried out. The spiteful person has an “accounting book” where they patiently hoard red numbers, waiting for the opportune moment to use them... They don't care much whether this time arrives, because ultimately they enjoy the unhappiness of the wait. In summary, good communication is derived from a proactive emotional style and poor communication from a reactive emotional style. We are going to study the latter.
Can you imagine being the doctor or nurse for a patient who you have a grudge against? That happens. This may originate from 'a trick' that the patient has played on us a few years ago. The consequences can be severe: blocking the relationship and preventing a genuine interest in what happens to the patient, our energy may be diverted to thinking about how much we wish to help the patient as a consequence of the grudge we hold against them. Even if the clinician thinks that they are doing 'as to any other patient', they run the risk of trivialising complaints: 'again as always, how annoying'. This is a high risk profile for clinical errors. Therefore, we must our cards on the table, and decide whether to continue the relationship or whether to break it. If we decide to continue with the relationship it is imperative to restart with a blank slate. Clearing our memory of unpleasant sequences encountered in our life is a basic mechanism to preserve the health of our personal relationships, which is almost as much as saying it is to preserve our mental health.
Another way that the clinician has of offloading their frustration is by humiliating the patient or their relatives. For example in paediatric emergencies:
- 'And why have you brought us the girl after waiting so many hours before coming here? Of course, as the football match has finished, you thought let's go all to A&E, didn’t you? If you were really sick, it would be different'.
- You don't do anything to lose weight and you just want tablets for it, but if you behave like this we are not going to get anywhere.
The same in a constructive tone:
- Of course, we will give you some medicine for your knee pain, but it will help if you can lose 5 or 10 kilos.
Contrary to poor communication (where guilt, humiliation and resentment are basic pillars), good communication is a cooperative type of communication. The concept of authority gives way to the concept of utility: being helpful to the patient even though we must try to rectify their behaviour. The key of this style lies in an emotional tone of accepting the other person, the integration of their expectations and empathy.
Accepting others
The patient does not need to present with an organic disease to be considered as a patient. Their concerns or discomfort are sufficient reasons. We're not going to criticise their personality or their way of being. People are as they are, and it is useless (when not counterproductive), to imagine a scenario of 'perfect' or 'good patients'. Good for whom? The clinician should accept the variety and richness of the human being. A difficult patient is a great opportunity to detect our technical and emotional shortcomings. Utopia (in reality dystopia) of 'the good patient' consists of a world full of educated polite citizens who provide well prepared reasons for consultation in a perfect expressive style, and with interesting illnesses. The utopia of ‘the good patient’ has done enormous harm to professionalism, and it spreads in an unapparent way from tutors to students or registrars.
Integration of expectations
Promoting their verbalisation is the first step, but it is not enough to only listen to them, we must address them. We address them when we say: 'I will take it into account', when we adapt the course of action to their preferences or when we advocate alternatives to give the patient a sense of control.
Empathy
We have talked about it, but here we want to emphasise its expressive component. There is at this point a lot of voluntary cleansing of our usual way of speaking. A patient is not tuberculous, but has tuberculosis, their anxieties are never nonsense, and their complaints are not, banalities. When we scrub this type of everyday expression we start to make empathy a habit (and we start to be better!) as rightly taught by Siddhartha Gautama 600 years BC [Smith H, 2002, p. 117].
Therapeutic commitment
Don't confuse the emotional quality of a relationship with therapeutic agreement. What we mean by therapeutic agreement (Shea SC, 2002) is the degree of risk, effort and even personal sacrifice to the patient, or in some cases the clinician, are willing to face in the therapeutic process. You can maintain good communication with the patient, but the therapeutic agreement can still be very scarce. Data to suspect a lack of therapeutic agreement:
-
Patient doesn't attend some of their appointments.
-
When the dialogue advances towards conflict situations one of the protagonists (the patient or the practitioner) diverts the conversation.
-
We detect a lack of adherence by the patient to the treatment or advice.
-
When the patient leaves the room, the practitioner feels the need to make a mocking comment to a colleague, or a student sitting in with them.
The reasons why a patient is not committed to the relationship may vary depending on the clinical situation or health problem. They may panic when they recognise the true nature of their family relationships, they may feel shame at having shown part of their intimate life, they may be suspicious that confidentiality won't be maintained, they may feel ashamed to show a part of their body... or their personality, or being dependent on others, etc.
On the professional side the problem is not so much related to confidence or modesty as laziness and risk. Therapeutic commitment is to take a x-ray and double-check it with a radiologist, or in the case of a nurse, request the patient waits a few minutes while they refer a question to the doctor, calling a specialist to get an urgent appointment, or discussing a significant event with the team where our performance was misguided or trying to get advice from colleagues to rectify an error.
Sometimes the patient literally 'surrenders' their privacy to the practitioner, even in a first visit. Warmth produces a false sense of familiarity in the patient, but this is not equivalent to a future commitment to the healthcare process, because amongst other reasons in the solitude of their home, they may experience a feeling of shame which prevents them from returning. Result: we have lost the patient. In this sense, when in a first interview the patient reveals very intimate aspects, it may be appropriate to tell them before closing the interview: 'how did you feel about telling me all this?'. If feelings of guilt or shame appear, you will work to try to normalise them: 'many people feel the same... what you have told me it is not unusual or strange. It is normal to feel shame from what you've told me. But remember that we have a duty of confidentiality'. And, finally, to minimise their reaction of shame: 'Let's arrange follow up another day... because I would like to assess the evolution of this problem’ (preferably when related to discomfort in a biological area).
The good listener
Byrne and Long (1984) in pioneering work with audiotape recordings, studied more than 2,000 interviews in primary care and they came to the conclusion that practitioners were leaning mainly to a style 'centred on interviewer's experience'. This would, on the one hand, note that the occupation of time, what we call today verbal occupation of the interview's time, was in favour of the practitioner. As a result, the patient could not express all their concerns. The interviewers allowed the patient to express a demand at the beginning of the consultation, but then the rest of the interview ran with a 'high control'. (Platt FW, 1979): the interviewer demarcated at every moment what they wanted the patient to tell them. In the Eurocommunication Study, mean verbal occupation from good interviewers ranged from 51 and 54% of the total time (van den Brink-Muinen, 1999).
Could it be a great waste of time if the patient expresses their self with absolute freedom? Does it involve real benefits? We advocate a moment in any interview which we call 'narrative support' or 'vanishing point', where we will proceed to the emptying of the pre-prepared information and listening without restrictions, where the practitioner should act as a mere support and offer encouragement.
Cordiality, together with reactivity, determines the amount of spontaneous information the patient produces. Empathy (already described sufficiently), determines the depth of the content. We understand the reactivity of the interviewer to be the time the interviewer takes to intervene after the patient has spoken. High reactivity means professional interruptions occur, and low reactivity means dysfunctional silences. Dysfunctional silence is one in which the patient expects the interviewer to say or do something (Froelich RE, 1977, p. 39). The discomfort of the patient falls on the interviewer. On the other hand, functional silences help the patient to concentrate, give them a space to think, or trigger tension which leads them to say or do something that they initially did not want to say or do. For example, this would be a dysfunctional silence:
Mother: There are these tummy pains which she has at school.
Paediatrician: Oh, well? (looking at the girl) I see, I see … (silence)
Mother (interrupting the silence): Could this be due to stress?
This silence is dysfunctional because it puts the focus on observing the girl, not on the girl to talk. The mother notices it and interrupts the silence. On the other hand this would be a functional silence:
Mother: There are these tummy pains which she has at school.
Paediatrician: Oh, well? (looking at the girl), let's see Olivia, what can you tell me about them? (bridge technique)
There is a silence that the paediatrician bears, looking at the girl with a smile. As you he can see the patient is not encouraged to speak, he continues:
Paediatrician (in a warm manner): Is there something in school that worries, or bothers you?
There is a new silence, which on this occasion the mother interrupts.
Mother: She has told me that there are some children who make fun of her when they have gymnastics, is that right Olivia?
Olivia crosses her arms and legs (closed body language), so the paediatrician prefers to reduce tension:
Paediatrician: Sometimes this happens and it is very unpleasant, so Olivia I understand you perfectly, if this is the case. We will nevertheless look at your tummy, come to the examination couch...
Another technique of less substance are the facilitations and the polite orders. The first is a behaviour of the interviewer, either verbal or non-verbal, which tries to help the patient to start or continue their story without indicating, suggesting or prejudging the contents of this. The interviewer may nod indicating to the patient 'continue, I am carefully listening to you' or make encouraging sounds of similar meaning. Other times the interviewer will demonstrate this with polite orders such as: 'I would like you to continue, please', 'is there anything else?', 'tell me more about that...'.
Interviewers with facilitation skills often use a mirror technique in which an emotional reaction similar to those experienced by the patient is reflected in the interviewers face. If the patient shows pain, the interviewer will make a micro-expression of pain, if the patient laughs, they will smile, etc. Notice how important it is to detect the asymmetric position (contrary to the mirror technique) in a conversation: we smile and the patient avoids eye contact or he clearly doesn't smile. This asymmetry clearly shows us that the patient isn't in emotional flow with us and that we do not have empathy or sympathy. Something is going on. Don't forget that communication is an eminently qualitative process in which this type of meaningful sign is significant. Accordingly, the mirror technique is based on correspondence: you give to me; I give to you; 'I have received the message and I understand it'. A brief frown with the eyebrows, a smile that means 'of course'', along with a low reactivity and functional silences, all of which make up the non-verbal dimension of a mirror technique. Therefore the mirror technique is more a consequence of the environment created than a specific technique.
Do not confuse facilitation with an initially facilitative sentence that ends with a question; for example: 'go on... did your leg hurt more at night?'. In this case the facilitation has no value, because the patient's attention will head for the final question. When two verbal techniques are juxtaposed, the value of the whole is usually that of the latter technique.
Reflecting back consists of repeating a word or a sentence that the patient has just said to direct their attention to that aspect. It has the great advantage that the patient cannot deny something that they have just said. If, for example, the patient says: 'all of this makes me feel bad, but one tries to live a normal life and forget', and we repeat: 'What makes you feel bad?', we will provoke the patient to access the memories which make them suffer, while if we say: 'you want to live a normal life', this sentence will facilitate the restructuring of their defences.
Sentences by repetition are very useful, provided we only use them occasionally. Being easy to do (just repeat what the patient has just said), we could be tempted to use them frequently, with the consequent fatigue (or even irritation) of the patient. As a rule, we recommend you use them at key moments of the interview, when we have the impression that the patient is saying something important and the same flow of ideas separates them from less interesting topics. It is worth notice that repetition should be done in an appropriate tone of voice. If, for example, the patient says: 'I can't work at all', and we repeat: 'at all?' incredulously, we have obviously asked an antagonistic question, rather than a sentence by repetition. Very close to this technique we have suggested addition: Add an adjective or a fact that we think the patient wishes to express, or is about to express.
Clarification is a verbal or non-verbal intervention which requires the patient to explain the meaning of a term or idea. For example: 'what do you mean by...?' or an equivalent expression requesting clarification. As we said before, it would be a mistake to abuse this technique, as we would give the impression of performing a police interrogation. We must also avoid using an inappropriate tone which makes it sound like implicit criticism.
The Signalling technique shows emotions or behaviour. This can be done with an observation of the patient's mood ('you look...') or a recent behaviour ('for a month I have seen that..'). The first is emotional signalling and second is behavioural signalling.
Signalling is equivalent to: 'seeing what is happening, or what is happening to you, what does it suggest?'. Needless to say it is a very powerful technique, to the extent that it can completely transform the healthcare relationship. Imagine the case of a patient coming to see the nurse as a follow up of her obesity, where the practitioner becomes aware of small signs of tension even hostility. At a given moment they say: 'lately I see you are very tense'. The effect is immediate: the patient looks downs and becomes tearful. A dysfunctional silence appears, because the patient is overwhelmed by emotion, the weight of it rests with the nurse which forces her to add: 'we can talk about it, if you think that will be helpful'. This comment is enough for the patient to explain her difficulties with her teenage daughter. From this point the goal is transformed: obesity ceases to have relevance and addressing the patient’s difficulties with her daughter becomes the focus of the consultation.
Beware of the iatrogenic effect of signalling. The typical case is when a practitioner discovers on a first visit the relationship between certain symptoms and a bereavement recently experienced by the patient. A signalling question such as: ‘your symptoms start precisely since the death of your family member, what does this suggest to you?’ This statement may be appropriate if made in a relationship sustained by confidence and therapeutic commitment, but it can have unpredictable effects on a first visit.
Some authors confuse signalling, empathy and interpretations (for example. making measurement of empathy by Carkhuff and Pierce [1975]). This can make the interviewer think that they are making an empathetic statement when in reality they are signalling, for example: ‘you are overwhelmed by being your mother’s carer, to the point that you have mixed feelings’. It would be interpretation if you add: ‘and this is because you see yourself alone with so much responsibility, and the rest of your brothers are not helping’ For LM Brammer (1985, pp. 84-86) a rainbow could be drawn from verbal interventions with signalling value to deep interpretations. Imagine that in the course of a conversation the patient tells us about his marriage difficulties. The three positions of the rainbow are exemplified follows. Signalling to the patient’s emotions: ‘but what feelings do you have towards your wife?’ signalling towards behaviour: ‘do you realise that you always need to blame her?’ Suggested interpretation: ‘does seeing her so independent make you feel uncomfortable?’ Finally, we would be interpreting if we were saying: ‘your marriage is filled with recriminations, it as if you act to harm each other harm’, and even deep interpretation if we assert: ‘you have a protective role towards her, but she wants to show you she is a free and autonomous person, and that you cannot easily accept that’.
We recommend rarely using suggested interpretations and almost never using interpretations. A way of doing it is to suggest our views and, whenever possible, express them as questions. For example: ‘it seems to me’ ‘I wonder if the fact that you drinking more alcohol could be related to ... ‘, ‘correct me if I'm wrong, but ...’ etc., ending with ‘It may be that … happens...’. Consider the following list:
|
|
|
|
|
|
|
|
|
With this gradation of techniques we will go at pace respectful to the patient’s needs and maturation (Balint M, 1971, p. 175). We have to say, in conclusion, that we have repeatedly seen the use of signalling and interpretations where the real goal was to confront, criticise, blame, or humiliate the patient. There is a key difference between confront and antagonising. Confrontation would be putting the patient against their reality to make them react positively. The purpose is to achieve mobilisation of their energy in a positive direction. For example: ‘we have to talk very seriously about your alcohol intake’. 'I think you are drinking again, is this right?' In contrast, antagonising is to criticise without suggesting an alternative behaviour. For example: 'you don't strive to take your pills because you hope your disease will resolve with herbal tea and quackery. All these alternative medicines you are taking are pure nonsense and ignorance'. Most antagonisms are carried out simply by how we pronounce a word. For example: ' I am very tired' and the practitioner responds with surprise and mockery: 'Yesss!'
The importance of non-verbal communication
Everything that is close we find strange, French philosopher Bataille G said (1975). Nothing is closer to oneself than the word, but not what we are trying to say with it, but its articulation. The human being is an Act. Habermas, for example, likes the term 'Act of communication' (Habermas J, 1999) to highlight this desire to communicate and to also emphasise the role of gesture that any snippet of communication has. Primarily, human communication is composed of gestures. Even when we think, we imagine ourselves in words or gestures, and if we pay attention to William James, when we think of words we don't stop articulating them in an imaginary way.
We understand non-verbal communication as a type of gesture, and as such it acquires the four values of any gesture:
-
Value of symbol: when it translates an exact meaning. It would be the case if we say 'yesss' as indicating 'are you sure?' No one would escape the symbolic intonation of this type.
-
Value of Illustrator: when it accompanies the meaning of the word to highlight it. For example: 'soooo big'.
-
Value of adapter: when it expresses unintentionally a state of anxiety or stress, or other emotion. Characteristic is the initial tremor in the speech of a speaker, which disappears as soon as they feel more comfortable.
-
Value of regulator: with the paralanguage we suggest... 'I'm going to finish speaking’, or 'you speak, please', and even 'I won't listen to you until I’ve finish speaking'.
Beyond these values, paralanguage informs us of the accent (local variety in the way of speaking), and tells us much about the person (Table 2.8), both in terms of their personality and character (Ethos, of Aristotle), as their ability to use the vocal features which accompany speech and contribute to communication to be heard and be better understood (pathos).
|
Table 2.8. What paralanguage tells us |
|
Structural Quality: accent, intonation and pronunciation of certain words. Personal Quality: pronunciation reactivity; use of silences (for example to give a dramatic quality) precision in the articulation of words, etc. Communication Quality: The tone and inflection of the voice, the use of silence, the articulation of silences, adjusting the volume to the situation and to the listener, pausing to allow understanding of what we are saying. The values of symbol, illustrator, adapter or regulator. Elocutionary force (see Glossary). Semiotic Quality of paralanguage: punctuated voice (for example, Parkinson’s), bitonal (for example, hypothyroidism), dysphonia (for example, due to swelling or polyps of the vocal cords), severe or acute tone (for example during puberty). |
The expert interviewer learns to take advantage of all this at two levels: a) to track the most imperceptible emotions of the patient, and b) to realise their own emotions. In the present work we extend the idea of William James as emotions form a steady stream of response to the environment. We are only aware of emotions which reach a certain threshold and have an impact of such force that they activate our body in a clear manner. We call these emotions 'fear', 'excitement', 'surprise', etc. But many other emotions are expressed as small fluctuations in bodily sweating, or a feeling of warmth in the abdomen or chest, without receiving a specific adjective. We could say that in their first stage emotions are variations of our attention, and when we are in a situation relevant, to this activation an interpretation is added which eventually gives the emotion a more precise meaning, suitable for an adjective, for example, fear, joy, surprise or the corresponding adjective to describe the emotion.
Paralanguage is sensitive to small emotional changes. Alongside the observation of perspiration (which is more difficult to notice without instrumental support), these are the two finest indicators to realise where our insignificant emotional changes are. We should bear in mind, according to James, that we are conscious of our emotions and give them a label when we interpret our bodily activation in a given environment. For example, when we notice our muscles are tense we will say 'I'm nervous'. In general, we put specific names to clusters of inner feelings. During this process we could be very ignorant to the point of being oblivious to almost all body emotions; or otherwise very sensitive amplifying the slightest reactions. Some people have, or they think they have good insight, i.e. a good capacity to understand their emotions and feelings. However, it may well be that some emotions could felt without the person realising it, and that they were giving the incorrect names to certain clusters of inner feelings. These are people who project a certain image of themselves onto how they really feel. Practicing complete transparency towards our own emotions is not easy, because who we are does not always match with who we want to be. This is a tension which has a rational explanation. Imagine a Kleptomaniac trying to suppress their impulse in a department store. Undoubtedly, by means of walking through different rows of objects without touching them, there will become a point where their compulsion will be partially wiped out. There is plasticity in our emotional reactions. But the first step of this virtuous Kleptomaniac will have been to honestly admit their drive, isolate it and neutralise it.
We suggest that the reader works on their insight on the basis of becoming fully transparent towards their reactions. For that one must overcome any temptation of hypocrisy towards oneself, which is not equivalent to being justified, but is to delay any judgment. All human beings experience emotional reactions which go against what we believe to be our nature. It is better to know this than to ignore it and ignore our emotions. In the field of professionalism which concerns us, we can experience a reaction of rejection or tiredness in situations which should inspire compassion and patience in us. In such circumstances, our true way of being is hidden by what we 'should be'. We do not allow ourselves to be transparent because this would damage our self-esteem and (more importantly), we should also modify our behaviour to be consistent. Listening to our paralanguage is a rich and accurate source which brings us closer to our hidden emotions, and to what we really feel. And, in the same way, refining our paralanguage forces us, as in the example above, to consult in a more patient manner, and in general to refocus our very primitive emotions. Re-education of paralanguage is to re-educate our feelings. Confucius, an expert in this, once exclaimed: ‘in my 70s I could follow what my heart desired without falling into any impropriety’ (J. Mosterin, 1997). Hopefully the reader will achieve this earlier.
Time management
And all we have seen... in just 10 minutes of an interview. It seems an impossible challenge, and partly it is for an inexperienced or unfocused clinician or a clinician with little psychological or physical reserve.
The most difficult thing is, having the ideal level of concentration every day to perform to the best of our ability. This claim of ‘giving the most of ourselves’ must not lead to ‘giving the maximum in every encounter and to every patient’. This is simply impossible, and it is because we have reserves of energy which need to last for the whole of the working day that we should calibrate our forces and manage them wisely.
What does ‘wisdom’ mean in this context? It means, basically:
-
Guessing the complexity of the clinical case and if necessary, changing the first time estimation we have made.
-
Knowing when we should accelerate the resolution of an interview and when we should slow it. Using a car analogy, when we need to move from ‘direct’ to ‘gear’.
Note reader, the amount of emotional ‘micro control’ we are investing in this whole process. On one hand, we must ‘get in tune’ when we begin the workday. We must ask ourselves: 'am I ok to start my clinic?’ ‘Perhaps, am I muddled? Or in a bad mood? And if the response is positive, we must implement various corrective mechanisms.
Time management is a major modulator of our emotionality. It requires firstly, patience. Patience is required when, for example, after we have prevented multiple additive requests a patient says: ‘what about my back pain?’ Patience is required when we are repeatedly interrupted by phone calls, patients or team mates coming into our room freely. An experienced clinician is not a clinician with many years of practice, but a professional who knows how to modulate their emotions linked to small gestures and daily events. It is a professional who knows adversities of ‘wanting at all costs to be able to have breakfast’, one who has made a mistake and who has learned from their mistakes. What's more, the mistakes have hurt them. The experience of making a mistake despite being a good professional and apparently having done ‘everything right’; puts the professional at a point of reflection and prudence that is the unmistakable sign of their maturity. When this stage is reached, the patients themselves notice it. There is a certainty tone complemented with humility, a tone that lets one say:
-
‘What you are telling me is important and deserves to be looked at in detail. What do you think if we arrange another visit for…?’
That tone provides a degree of freedom to the clinician: to lengthen an interview when it is seemingly finished, to conclude it quickly when the demand is trivial. In short, give rationally, the necessary effort to meet each demand.
Bibliography
Balint M. El médico, el paciente y la enfermedad. Buenos Aires: Libros Básicos, 1971. Bataille G. La experiencia interior. Madrid: Taurus, 1975.
Beach LR. Image Theory: Decision making in personal and organizational contexts. Chichester, UK: Wiley, 1990.
Bennet MJ. Overcoming the Golden Rule: Simpathy and empathy. En: Bennet MJ. Basic Concepts of Intercultural Communications. Maine: Intercultural Press, 1998.
Bernstein L, Bernstein RS. Interviewing. A guide for health professionals. Norwalk, Connecticut: Prentice-Hall Inc., Appleton Century Crofts,1985.
Borrell F. Cómo trabajar en equipo. Barcelona: Gestión 2000, 2001. Borrell F. Manual de Entrevista Clínica. Barcelona: Doyma, 1989.
Borrell F, Núñez B, Guerrero J, Babi P, Navarro J, Alvarado CE. Auditoría de las Historias Clínicas de Atención Primaria: 6 años de experiencia. Gaceta Sanitaria 1988; 6(2): 144-149.
Borrell F. El problema no és el paternalisme, el problema és la fredor del tècnic. Comunicación Congreso Salut Mental Atenció Primaria, SCMFC, Fundació Salut Mental. Badalona, 14-15 marzo 2002, «Canviant la mirada». Badalona 2002, págs. 11-13.
Brammer LM. The helping relationship: process and skills. Londres: Prentice-Hall International Editions, 1985, págs. 84-86.
Brown JB, Stewart MA, McCracken EC, McWhinney IR, Levenstein JH. The patient-centred clinical method II. Definition and application. Fam Pract 1986; 3: 75-79.
Byrne PS, Long BEL. Doctors Talking to Patients. Londres: Her Majesty’s Stationary Office, 1976. Camps V. Una vida de calidad. Barcelona: Ares y Mares, 2001, págs. 184-186.
Carkhuff RR, Pierce RM. Trainer’s guide. The art of helping. Massachussets: Human Resource Development Press, 1975.
Cohen-Cole SA. The Medical Interview: the three-function approach. Sant Louis: Mosby, 1991. Coulehan JL, Block MR. The Medical Interview. Mastering Skills for Clinical Practice. Filadelfia: FA Davis Company, 1997
Duck S, Gilmour R. Personal Relationships. Londres: Academic Press, 1981, pág. 42.
Emanuel EJ, Emanuel LL. Cuatro modelos de la relación médico-paciente. En: Azucena Couceiro (ed.). Bioética para clínicos. Madrid: Triacastela, 1999.
Feinstein A. Clinical Judgment. Baltimore: Williams and Wilkins, 1967.
Fernández Liria A. Conceptos sustantivo y pragmático de la enfermedad mental. Implicaciones clíni- cas. En: Baca E, Lázaro J. (eds.). Hechos y valores en psiquiatría. Madrid: Triacastela, 2003.
Froelich RE, Bishop FM. Clinical Interviewing Skills. Saint Louis: The CV Mosby Company, 1977. Habermas J. Teoría de la acción comunicativa. Tomos I y II. México DF: Taurus, 1999.
Headington BJ. Communications in the counseling relationship. Cranston: The Carroll Press, 1979, págs. 64 y 72.
Guillem Salvador. Comunicació a la Mesa: Relació metge-pacient, canvis i reptes. Congrés Salut Mental Badalona, 2002.
Goleman D. Inteligencia emocional. Barcelona: Kairós, 1996.
Laín Entralgo P. La relación médico-enfermo. Historia y Teoría. Revista de Occidente. Madrid, 1964. Mosterín J. Historia de la Filosofía. La filosofía oriental antigua. Madrid: Alianza Editorial, 1997, pág. 119.
Peabody FW. The care of the patient. JAMA 1984; 252(6): 813-818.
Platt F. Patience. Health and Communication International Conference. Barcelona: Universitat Pompeu Fabra, 2000.
Platt FW, McMath JC. Clinical hypocompetence: the interview. Ann Intern Med 1979; 91: 898-902.
Rogers C. El poder de la persona. México: El Manual Moderno, 1980. Rubert de Ventós X. Ética sin atributos Barcelona: Anagrama, 1996. Sádaba J. El hombre espiritual. Barcelona: Martínez Roca, 1999.
Shea SC. La entrevista psiquiátrica. El arte de comprender. Madrid: Harcourt, Saunders Elsevier Sciences, 2002.
Smith H. Las religiones del mundo. Barcelona: Kairós, 2002.
Stewart MA. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med 1984; 19(2): 167-175.
Suchman AL, Bothelo RJ, Hinton-Walker P. Partnerships in Health Care. Transforming relational process. Rochester: University of Rochester, 1998.
Tizón J. Componentes psicológicos de la práctica médica. Barcelona: Doyma, 1988
Tizón T. Apuntes para una psicología basada en la relación. Barcelona: Hora, 1982.
van den Brink-Muïnen, Verhaak PFM, Bensing JM et al. The Eurocommunication Study. Utrecht: Nivel, 1999.